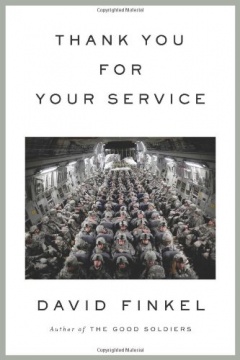
Brain Wars: How the Military is Failing its Wounded
This comprehensive multimedia investigation delves into the ramifications of the signature wound of today’s wars: traumatic brain injury (TBI). Originally published by ProPublica and NPR in 2010.
Brain Injuries Remain undiagnosed in Thousands of Soldiers
WASHINGTON, D.C.--The military medical system is failing to diagnose brain injuries in troops who served in Iraq and Afghanistan, many of whom receive little or no treatment for lingering health problems, an investigation by ProPublica and NPR has found.
So-called mild traumatic brain injury has been called one of the wars' signature wounds. Shock waves from roadside bombs can ripple through soldiers' brains, causing damage that sometimes leaves no visible scars but may cause lasting mental and physical harm.
Officially, military figures say about 115,000 troops have suffered mild traumatic brain injuries since the wars began. But top Army officials acknowledged in interviews that those statistics likely understate the true toll. Tens of thousands of troops with such wounds have gone uncounted, according to unpublished military research obtained by ProPublica and NPR.
"When someone's missing a limb, you can see that," said Sgt. William Fraas, a Bronze Star recipient who survived several roadside blasts in Iraq. He can no longer drive, or remember simple lists of jobs to do around the house. "When someone has a brain injury, you can't see it, but it's still serious."
In 2007, under enormous public pressure, military leaders pledged to fix problems in diagnosing and treating brain injuries. Yet despite the hundreds of millions of dollars pumped into the effort since then, critical parts of this promise remain unfulfilled.
Over four months, we examined government records, previously undisclosed studies, and private correspondence between senior medical officials. We conducted interviews with scores of soldiers, experts and military leaders.
Among our findings:
- From the battlefield to the home front, the military's doctors and screening systems routinely miss brain trauma in soldiers. One of its tests fails to catch as many as 40 percent of concussions, a recent unpublished study concluded. A second exam, on which the Pentagon has spent millions, yields results that top medical officials call about as reliable as a coin flip.
- Even when military doctors diagnose head injuries, that information often doesn't make it into soldiers' permanent medical files. Handheld medical devices designed to transmit data have failed in the austere terrain of the war zones. Paper records from Iraq and Afghanistan have been lost, burned or abandoned in warehouses, officials say, when no one knew where to ship them.
- Without diagnosis and official documentation, soldiers with head wounds have had to battle for appropriate treatment. Some received psychotropic drugs instead of rehabilitative therapy that could help retrain their brains. Others say they have received no treatment at all, or have been branded as malingerers.
In the civilian world, there is growing consensus about the danger of ignoring head trauma: Athletes and car accident victims are routinely tested for brain injuries and are restricted from activities that could result in further blows to the head.
But the military continues to overlook similarly wounded soldiers, a reflection of ambivalence about these wounds at the highest levels, our reporting shows. Some senior Army medical officers remain skeptical that mild traumatic brain injuries are responsible for soldiers' troubles with memory, concentration and mental focus.
Civilian research shows that an estimated 5 percent to 15 percent of people with mild traumatic brain injury have persistent difficulty with such cognitive problems.
"It's obvious that we are significantly underestimating and underreporting the true burden of traumatic brain injury," said Maj. Remington Nevin, an Army epidemiologist who served in Afghanistan and has worked to improve documentation of TBIs and other brain injuries. "This is an issue which is causing real harm. And the senior levels of leadership that should be responsible for this issue either don't care, can't understand the problem due to lack of experience, or are so disengaged that they haven't fixed it."
When Lt. Gen. Eric Schoomaker, the Army's most senior medical officer, learned that NPR and ProPublica were asking questions about the military's handling of traumatic brain injuries, he initially instructed local medical commanders not to speak to us.
"We have some obvious vulnerabilities here as we have worked to better understand the nature of our soldiers' injuries and to manage them in a standardized fashion," he wrote in an e-mail sent to bases across the country. "I do not want any more interviews at a local level."
When confronted with the findings later, however, he acknowledged shortcomings in the military's diagnosing and documenting of head traumas.
"We still have a big problem and I readily admit it," said Schoomaker, the Army's surgeon general. "That is a black hole of information that we need to have closed."
Brig. Gen. Loree Sutton, who oversees brain injury issues for the Pentagon, said the military had made great strides in improving attitudes towards the detection and treatment of traumatic brain injury.
The military is considering implementing a new policy to mandate the temporary removal from the battlefield of soldiers exposed to nearby blasts. Later this year, the Pentagon expects to open a cutting-edge center for brain and psychological injuries, which will treat about 500 soldiers annually.
"This journey of cultural transformation, it is a journey not for the faint of heart," Sutton said. "At the end of our journeys, at the end of our travels, what we must ensure is, we must ensure that we have consistent standards of excellence across the board. Are we there yet? Of course we're not there yet."
Soldiers like Michelle Dyarman wonder what's taking so long. Dyarman, a former major in the Army reserves, was involved in two roadside bomb attacks and a Humvee accident in Iraq in 2005.
Today, the former dean's list student struggles to read a newspaper article. She has pounding headaches. She has trouble remembering the address of the farmhouse where she grew up in the hills of central Pennsylvania.
For years, Dyarman fought with Army doctors who did not believe that she was suffering lasting effects from the blows to her head. Instead, they diagnosed her with an array of maladies from a headache syndrome to a mood disorder.
"One of the first things you learn as a soldier is that you never leave a man behind," said Dyarman, 45. "I was left behind."
In 2008, after Dyarman retired from the Army, Veterans Affairs doctors linked her cognitive problems to her head traumas.
Dyarman has returned to her civilian job inspecting radiological devices for the state, but colleagues say she turns in reports with lots of blanks; they cover for her.
Dyarman's 67-year-old father, John, looks after her at home, balancing her checkbook, reminding her to turn the oven on before cooking. The joyful, bright child he raised, the first in the family to attend college, is gone, forever gone.
"It hurts me, too," he said, growing upset as he spoke. "That's my daughter sitting there, all screwed up. She's not the kid she was."
Walkie Talkies
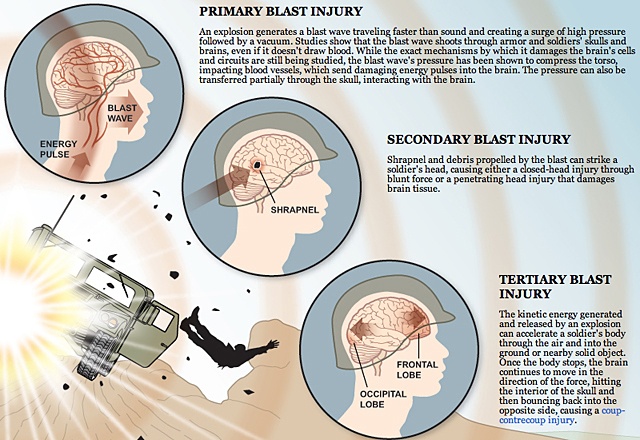
Better armor and battlefield medicine mean troops survive explosions that would have killed an earlier generation. But blast waves from roadside bombs, insurgents' most common weapon, can still damage the brain.
The shock waves can pass through helmets, skulls and through the brain, damaging its cells and circuits in ways that are still not fully understood. Secondary trauma can follow, such as sending a soldier tumbling inside a vehicle or hurling into a wall, shaking the brain against the skull.
Not all brain injuries are alike. Doctors classify them as moderate or severe if patients are knocked unconscious for more than 30 minutes. The signs of trauma are obvious in these cases and medical scanning devices, like MRIs, can detect internal damage.
But the most common head injuries in Iraq and Afghanistan are so-called mild traumatic brain injuries. These are harder to detect. Scanning devices available on the battlefield typically don't show any damage. Recent studies suggest that breakdowns occur at the cellular level, with cell walls deteriorating and impeding normal chemical reactions.
Doctors debate how best to categorize and describe such injuries. Some say the term mild traumatic brain injury best describes what happens to the brain. Others prefer to use concussion, insisting the word carries less stigma than brain injury.
Whatever the description, most soldiers recover fully within weeks, military studies show. Headaches fade, mental fogs clear and they are back on the battlefield.
For a minority, however, mental and physical problems can persist for months or years. Nobody is sure how many soldiers who suffer mild traumatic brain injury will have long-term repercussions. Researchers call the 5 percent to 15 percent of civilians who endure persistent symptoms the "miserable minority."
A study published last year in the Journal of Head Trauma Rehabilitation found that, of the 900 soldiers in one battle-hardened Army brigade who suffered brain injuries, most of them mild, almost 40 percent reported having at least one symptom weeks or months later.
The long-term effects of mild traumatic brain injuries can be devastating, belying their name. Soldiers can endure a range of symptoms, from headaches, dizziness and vertigo to problems with memory and reasoning. Soldiers in the field may react more slowly. Once they go home, some commanders who led units across battlefields can no longer drive a car down the street. They can't understand a paragraph they have just read, or comprehend their children's homework. Fundamentally, they tell spouses and loved ones, they no longer think straight.
Such soldiers are sometimes called "walkie talkies" -- unlike comrades with missing limbs or severe head wounds, they can walk and talk. But the cognitive impairments they face can be severe.
"These are people who go on to live" with "a lifelong chronic disability," said Keith Cicerone, a leading researcher in the field. "It is going to be terrifically disruptive to their functioning."
An increasing number of brain-injury specialists say the best way to treat patients with lasting symptoms is to get them into cognitive rehabilitation therapy as soon as possible. That was the consensus recommendation of 50 civilian and military experts gathered by the Pentagon in 2009 to discuss how to treat soldiers.
Such therapy can retrain the brain to compensate for deficits in memory, decision-making and multitasking.
A soldier whose injuries are not diagnosed or documented misses out on the chance to get this level of care -- and the hope for recovery it offers, say veterans advocates, soldiers and their families.
"Talk is cheap. It is easy to say we honor our servicemen," said Cicerone, who has helped the military develop recommendations for appropriate treatments for soldiers with brain injuries. "I don't think the services that we are giving to those servicemen honors those servicemen."
Missing Records
The military's handling of traumatic brain injuries has drawn heated criticism before.
ABC News reporter Bob Woodruff chronicled the difficulties soldiers faced in getting treatment for head traumas after recovering from one himself, suffered in a 2006 roadside bombing in Iraq. The following year, a Washington Post series about substandard conditions at Walter Reed Army Medical Hospital described the plight of several soldiers with brain injuries.
Members of Congress responded by dedicating more than $1.7 billion to research and treatment of traumatic brain injury and post-traumatic stress, a psychological disorder common among soldiers returning from war. They passed a law requiring the military to test soldiers' cognitive functions before and after deployment so brain injuries wouldn't go undetected.
But leaders' zeal to improve care quickly encountered a host of obstacles. There was no agreement within the military on how to diagnose concussions, or even a standardized way to code such incidents on soldiers' medical records.
Good intentions banged up against the military's gung ho culture. To remain with comrades, soldiers often shake off blasts and ignore symptoms. Commanders sometimes ignore them, too, under pressure to keep soldiers in the field. Medics, overwhelmed with treating life-threatening injuries, may lack the time or training to recognize a concussion.
The NPR and ProPublica investigation, however, indicates that the military did little to overcome those battlefield hurdles. They waited for soldiers to seek medical attention, rather than actively seeking to evaluate those in blasts.
The military also has repeatedly bungled efforts to improve documentation of brain injuries, the investigation found.
Several senior medical officers said soldiers' paper records were often lost or destroyed, especially early in the wars. Some were archived in storage containers, then abandoned as medical units rotated out of the war zones.
Lt. Col. Mike Russell, the Army's senior neuropsychologist, said fellow medical officers told him stories of burning soldiers' records rather than leaving them in Iraq where anyone might find them.
"The reality is that for the first several years in Iraq everything was burned. If you were trying to dispose of something, you took it out and you put it in a burn pan and you burned it," said Russell, who served two tours in Iraq. "That's how things were done."
To improve recordkeeping, medics began using pricey handheld devices to track injuries electronically. But they often broke or were unable to connect with the military's stateside databases because of a lack of adequate Internet bandwidth, said Nevin, the Army epidemiologist.
"These systems simply were not designed for war the way we fight it," he said.
In 2007, Nevin began to warn higher-ups that information was being lost. His concerns were ignored, he said. While communications have improved in Iraq, Afghanistan remains a concern.
That same year, clinicians interviewed soldiers about whether they had suffered concussions for an unpublished Army analysis, which was reviewed by NPR and ProPublica. They found that the military files showed no record of concussions in more than 75 percent of soldiers who reported such injuries to the clinicians.
Nevin said that without documentation of wounds, soldiers could have trouble obtaining treatment, even when they report they can't think, or read, or comprehend instructions normally anymore.
Doctors might say, "there's no evidence you were in a blast," Nevin said. "I don't see it in your medical records. So stop complaining."
Problems documenting brain injuries continue.
Russell said that during a tour of Iraq last year, he examined five soldiers the day after they were injured in a January 2009 rocket attack. The medical staff had noted shrapnel injuries, but Russell said they failed to diagnose the soldiers' concussions.
The symptoms were "classic," Russell said. The soldiers had "dazed" expressions, and were slow to respond to questions.
"I found out several of them had significant gaps in their memory," Russell said. "It wasn't clear how long they were unconscious for, but the last thing they remember is they were playing video games. The next thing they remember, they are outside the trailer."
Another doctor told NPR and ProPublica of finding soldiers with undocumented mild traumatic brain injuries in Afghanistan as recently as February 2010.
"It's still happening, there's no doubt," said the military doctor, who did not want to be named for fear of retribution
Screened Out
After the Walter Reed scandal, the military instituted a series of screens to better identify service members with brain injuries. Soldiers take an exam before deploying to a war zone, another after a possible concussion in theater, and a third after returning home.
But each of these screens has proved to have critical flaws.
The military uses an exam called the Automated Neuropsychological Assessment Metrics, or ANAM, to establish a baseline for soldiers' cognitive abilities. The ANAM is composed of 29 separate tests that measure reaction times and reasoning capabilities. But the military, looking to streamline the process, decided to use only six of those tests.
Doubts immediately arose about the exam, which had never been scientifically validated. Schoomaker, the Army surgeon general, recently told Congress that the ANAM was "fraught with problems" and that "as a screening tool," it was "basically a coin flip."
Military clinicians have administered the exam to more than 580,000 soldiers, costing the military millions of dollars per year, but have accessed the results for diagnostic purposes only about 1,500 times.
Rep. Bill Pascrell Jr., D-N.J., who has led efforts to improve the treatment and study of brain injuries, accused the military of ignoring the Congressional directive.
"We are not doing service to our bravest," Pascrell said. "There needs to be a sense of urgency on this issue. We are not doing justice."
Once in theater, soldiers are supposed to take the Military Acute Concussion Evaluation, or MACE, to check for cognitive problems after blasts or other blows to the head.
But in interviews, soldiers said they frequently gamed the test, memorizing answers beforehand or getting tips from the medics who administer it.
Just last summer, Sgt. Victor Medina was leading a convoy in southern Iraq when a roadside bomb exploded. He was knocked unconscious for 20 minutes.
Afterwards, Medina had trouble following what other soldiers were saying. He began slurring his words. But he said the medic helped him to pass his MACE test, repeating questions until he answered them correctly.
"I wanted to be back with my soldiers," he said. "I didn't argue about it.".
Senior military officials said problems with the MACE were common knowledge.
"There's considerable evidence that people were being coached or just practicing," said Russell, the senior neuropsychologist. "They don't want to be sidelined for a concussion. They don't want to be taken out of play."
If cases of brain trauma get past the battlefield screen, a third test -- the post-deployment health assessment, or PDHA -- is supposed to catch them when soldiers return home.
But a recent study, as yet unpublished, shows this safety net may be failing, too.
When soldiers at Fort Carson, Colo., were given a more thorough exam bolstered by clinical interviews, researchers found that as many as 40 percent of them had mild traumatic brain injuries that the PDHA had missed.
In a 2007 e-mail, a senior military official bluntly acknowledged the shortcomings of PDHA exams, describing them as "coarse, high-level screening tools that are often applied in a suboptimal assembly line manner with little privacy" and "huge time constraints."
Col. Heidi Terrio, who carried out the Fort Carson study, said the military's screens must be improved.
"It's our belief that we need to document everyone who sustained a concussion," she said. "It's for the benefit of the Army and the benefit of the family and the soldier to get treatment right away."
Gen. Peter Chiarelli, the Army's second in command, acknowledged that the military has not made the progress it promised in diagnosing brain injuries.
"I have frustration about where we are on this particular problem," Chiarelli said.
Fundamentally, he said, soldiers, military officers and the public needed to take concussions seriously.
"We've got to change the culture of the Army. We've got to change the culture of society," he said, adding later, "We don't want to recognize things we can't see."
Skeptics
The shift Chiarelli envisions may be impossible without buy-in from senior military medical officials, some of whom are skeptical about the long-term harm caused by mild traumatic brain injuries.
One of Schoomaker's chief scientific advisors, retired Army psychiatrist Charles Hoge, has been openly critical of those who are predisposed to attribute symptoms like memory loss and concentration problems to mild traumatic brain injury.
In 2009, he wrote a opinion piece in the New England Journal of Medicine that said the "illusory demands of mild TBI" might wind up hobbling the military with high costs for unnecessary treatment. Recently, Hoge questioned the importance of even identifying mild traumatic brain injury accurately.
"What's the harm in missing the diagnosis of mTBI?" he wrote to a colleague in an April 2010 e-mail obtained by NPR and ProPublica. He said doctors could treat patients' symptoms regardless of their underlying cause.
In an interview, Hoge said, "I've been concerned about the potential for misdiagnosis, that symptoms are being attributed to mild traumatic brain injury when in fact they're caused by other" conditions. He noted that a study he conducted, published in the New England Journal of Medicine, "found that PTSD really was the driver of symptoms. That doesn't mean that mTBI isn't important. It is important. It's very important."
Other experts called Hoge's posture toward mild TBI troubling.
To be sure, brain injuries and PTSD sometimes share common symptoms and co-exist in soldiers, brought on by the same terrifying events. But treatments for the conditions differ, they said. A typical PTSD program, for instance, doesn't provide cognitive rehabilitation therapy or treat balance issues. Sleep medication given to someone with nightmares associated with PTSD might leave a brain-injured patient overly sedated, without having a therapeutic effect.
"I'm always concerned about people trivializing and minimizing concussion," said James Kelly, a leading researcher who now heads a cutting-edge Pentagon treatment center for traumatic brain injury. "You still have to get the diagnosis right. It does matter. If we lump everything together, we're going to miss the opportunity to treat people properly."
***
At her family farm outside Hanover, Pa., Michelle Dyarman has a large box overflowing with medical charts, letters and manila envelopes. They are the record of her fight over the past five years to get diagnosis and treatment for her traumatic brain injury.
After her last roadside blast in Baghdad, which killed two colleagues, Dyarman wound up at Walter Reed for treatment of post-traumatic stress.
Over the course of two and a half years, she received drugs for depression and nightmares. She got physical therapy for injuries to her back and neck. A rehabilitation specialist gave her a computer program to help improve her memory.
But it wasn't until she began talking with fellow patients that she heard the term mild traumatic brain injury. As she began to research her symptoms, she asked a neurologist whether the blasts might have damaged her brain.
Records show the neurologist dismissed the notion that Dyarman's "minor head concussions" were the source of her troubles, and said her symptoms were "likely substantially attributable" to PTSD and migraine headaches.
"It was disappointing," she said. "It felt like nobody cared."
When she was later given a diagnosis of traumatic brain injury by Veterans Affairs doctors, she said she felt vindicated, yet cheated all at once.
"I always put the military first, even before my family and friends. Now looking back, I wonder if I did the right thing," she said. "I served my country. Now what's my country doing for me?"
After Our Investigation, Pentagon Puts Its Spin on Brain Injuries
ProPublica and NPR reported today that the military is failing to diagnose soldiers who suffered brain injuries in Iraq and Afghanistan. It didn't take long to get a response. Soon after learning that the stories were about to air, the Pentagon's public affairs machine began circulating talking points on traumatic brain injuries2014just in case senior medical commanders weren't up to speed on what the military's been doing for troops with one of the wars' signature wounds.
The talking points, which we obtained and were sent to top Army officials, don't directly address the findings of our investigation. We found that the military's system has repeatedly overlooked soldiers with so-called mild traumatic brain injuries. These blast injuries, which some doctors call concussions, leave no visible scars but can cause lasting physical and mental harm in some cases. The Pentagon's official figures say about 115,000 soldiers have suffered a mild traumatic brain injury since the wars began. But we found that military doctors and screening tools routinely miss soldiers who have suffered mild traumatic brain injuries on the battlefield. Experts we interviewed and documents we obtained said the military's count may understate the true toll by tens of thousands of soldiers.
The talking points are upbeat. One says that the Department of Defense has the "world's best TBI medical care for our service members." Leading neuropsychologists and rehabilitation therapists have told us that's not true, however. They say the military doesn't always provide the kind of intensive cognitive rehabilitation therapy most experts recommend. The talking points also stressed that one military screen, called the ANAM, for Automated Neuropsychological Assessment Metrics, will be "utilized when soldiers come home to help measure the effects of any identified mild brain trauma that may have gone unnoticed or untreated."
But when we talked to the man who ran that program, he told us the ANAM was rarely used that way. Lt. Col. Mike Russell, the Army's senior neuropsychologist, said that more than 580,000 ANAM tests have been administered to soldiers before they deploy to the battlefield. But doctors have only used them about 1,500 times to diagnose soldiers after they've suffered a blow to the head.
The talking points tick off a number of initiatives the military has undertaken to better diagnose and treat the soldiers. But as we note in our stories, the problem is not the lack of initiatives, it's that nine years into the war, nobody at the Pentagon knows how big the problem is, nor how best to treat it. You can find the complete talking points memos and PowerPoint here.
Phone calls to the medical command's spokeswoman were not immediately returned.
At Fort Bliss, Brain Injury Treatments Can Be as Elusive as Diagnosis
A version of this story was aired on NPR's "All Things Considered." Listen to the audio broadcast below:
FORT BLISS, Texas -- At this rapidly expanding base along the U.S.-Mexico border, the military is racing to build new homes for 10,000 additional soldiers. Cranes stack prefabricated containers like children's blocks to erect barracks overnight. Bulldozers grind sagebrush desert into roads and runways.
Just down the street from the construction boom squats a tan, featureless building about the size of a convenience store. Completed nearly a year ago, it remains unopened, the doors locked.
Building 805 was supposed to house a clinic for traumatic brain injury, often called the signature wound of the wars in Iraq and Afghanistan. Instead, it has become a symbol for soldiers here of what they call commanders' indifference to their problems.
"The system here has no mercy," said Sgt. Victor Medina, a decorated combat veteran who fought to receive treatment at Fort Bliss after suffering a brain injury during a roadside blast in Iraq last June. Since the explosion, Medina has had trouble reading, comprehending and doing simple tasks. "It's struggle after struggle."
Previously, ProPublica and NPR reported that the military has failed to diagnose brain injuries in troops who served in Iraq and Afghanistan. Mild traumatic brain injuries, which doctors also call concussions, do not leave visible scars but can cause lasting mental and physical problems.
At Fort Bliss, we found that even soldiers who are diagnosed with such injuries often do not receive the treatment they need.
Most specialists say it is critical for patients who show lingering effects from head trauma to get intensive therapy as soon as possible. In the civilian world, such therapy is increasingly seen as the best way to minimize permanent damage, helping to retrain the mind to compensate for deficits.
Yet brain-injured soldiers at Fort Bliss have had to wait weeks and sometimes months just to get appointments with doctors, medical records show. Many have received far less therapy than is typical at well-regarded civilian clinics. In some instances, Fort Bliss medical officers have suggested that the soldiers are malingerers or that the main root of their cognitive problems is psychological.
"Here you have all these soldiers looking for help, and it was just getting swept under the carpet," said Sgt. Brandon Sanford, 28, a dog handler who survived two roadside blasts in Iraq. Sanford endured a year of balance problems and mental fog before Fort Bliss officials sent him for cognitive therapy. "I served my country. I've got an injury to prove it."
It is impossible for civilians to know how Fort Bliss' care for brain-injured soldiers compares in quality or scale to that of other bases. Base officials would not give ProPublica and NPR data on how many soldiers are being treated there and the Pentagon would not provide this information for bases elsewhere.
Fort Bliss -- the third-largest base in the U.S. military and a vital nerve center for deploying and returning troops -- is supposed to be among the best. In 2007, the Pentagon designated it as one of 20 bases nationally that would develop augmented treatment programs for traumatic brain injury.
Yet while base commanders have spent more than $3 billion to expand and improve Fort Bliss over the past several years, they have directed just $5 million to facilities and clinicians to treat TBI. The program had no full-time director until October 2009. A neuropsychologist was hired only recently, after a two-year search.
Fort Bliss' commander, Maj. Gen. Howard Bromberg, declined repeated requests for an interview. Col. James Baunchalk, the base hospital's commander, acknowledged that the TBI program had encountered some delays, but said that it now had 12 clinicians -- four full-time and eight part-time -- who were delivering comprehensive care.
"I honestly believe that we've done a good job of meeting the needs for the community," Baunchalk said.
He promised in April that Building 805 would open by the end of May, saying they were just waiting until computer cabling was installed.
Apparently, they missed their deadline. As of early June, the clinic to screen soldiers for traumatic brain injury had not opened its doors to a single patient.
The Soldiers
Traumatic brain injuries are among the most common wounds sustained in Iraq and Afghanistan. Shock waves from bombs can pass through helmets and through the brain. Secondary trauma can occur when soldiers are thrown up against vehicles or walls, shaking the brain again.
Officially, the military says about 150,000 soldiers have suffered some form of brain injury since the wars began. But a 2008 Rand study suggests the toll is much higher, perhaps more than 400,000 troops. The most common type are so-called mild traumatic brain injuries. Most people recover quickly from such injuries, but studies have shown between 5 percent and 15 percent of patients may suffer long-term problems.
ProPublica and NPR interviewed more than a dozen soldiers at Fort Bliss who are among that so-called miserable minority. All were diagnosed by military doctors with at least one mild traumatic brain injury. All had persistent symptoms, ranging from headaches and vertigo to difficulties with memory and reasoning.
They described the bewildering ways in which their injuries had changed them. A sergeant who once commanded 60 men in battle got lost in a supermarket. A soldier who once plotted sniper attacks could no longer assemble a bird house. Most of them did not want their names used, for fear of harm to their military careers.
All felt the treatment they received was inadequate. At leading neurocognitive rehabilitation centers, some patients with mild traumatic brain injury often receive three to six hours a day of therapy for months from teams of highly trained specialists.
By contrast, many soldiers at Fort Bliss attended two to four hours of cognitive treatment per week. For some soldiers, weeks passed by with little or no treatment. The therapists who provided the soldiers with speech and occupational therapy for their brain injuries sometimes had only minimal training in cognitive rehabilitation, records show.
Staffing shortfalls also meant soldiers had long waits before beginning rehabilitative therapies. While clinical research is still developing, the consensus recommendation of a group of military and civilian experts convened by the Pentagon last year was to provide rehabilitation therapy as promptly as possible.
"The longer you go without therapy, the greater likelihood there is of falling into what I would call a mental disuse syndrome, where the brain is not being used at the same level," said Keith Cicerone, a leading rehabilitation researcher and the director of neuropsychology at the JFK Johnson Rehabilitation Institute in New Jersey. The brain "is in essence going to develop bad habits."
Sgt. Raymond Hisey, 32, a convoy driver in the 1st Armored Division, survived a roadside blast in Iraq in July 2009. He remained in the field, but endured constant headaches and balance problems. His short-term memory suffered and he struggled to think of words to express himself.
When he returned to Fort Bliss in October, he was diagnosed as having suffered a mild traumatic brain injury and was prescribed several courses of therapy. But a speech therapist cancelled several appointments, he said, and he clashed with the occupational therapist. Hisey was suddenly left without any treatment at all for his symptoms.
"You just get lost in the system," he said. "I could have pushed more, sure. But people kept saying it gets better over time. I thought I was just losing my damn mind, to be honest with you."
Fort Bliss is supposed to provide treatment to troops at smaller bases in the surrounding area. But one such soldier who developed headaches and balance problems after working on a mining detail in Afghanistan was told that no therapists could make regular trips to see him. Instead, the soldier, whose base was about an hour away from Ft. Bliss, was given antidepressants, which he did not take. He recently deployed for a second tour.
"As much as the military is making of TBI and the effects it's having on the soldiers and their families, I think for something as big as Fort Bliss, there'd be more people" to treat it, said the soldier, a specialist who did not want his name used for fear of damaging his career. "I was told there were no resources, no facilities."
Baunchalk, the hospital commander, said he had never heard such complaints from soldiers or their spouses. Soldiers were often reluctant to seek care, he said, because they perceived a stigma attached to traumatic brain injury.
"It's tough for them to step forward and say ... I need some help," he said. "I don't think we have that many soldiers who have fallen through the cracks."
Several soldiers told ProPublica and NPR, however, that they and their families had reached out to base commanders, sent e-mails to generals throughout the Pentagon, and even written to members of Congress, pleading for care.
When their efforts proved futile, they felt abandoned. Nobody paid attention, they said, to a soldier with an injury that nobody could see.
"No one listens to the soldier," said Sgt. William Fraas, an 18-year military veteran and Bronze Star recipient who struggled for nearly two years to get help for problems with his balance and vision. "They are there and they are crying for help."
The Neurologist
Fort Bliss soldiers struggling with the effects of brain injuries were often sent to the base's sole neurologist, Capt. Brett Theeler. Theeler, records show, sometimes blamed psychological disorders rather than blast wounds as the likely source of soldiers' cognitive problems.
A convoy commander in the 121st Brigade of the 1st Armored Division, Sgt. Victor Medina can see the moment he suffered his invisible injury. He was rumbling down a highway in southern Iraq June 2009 in a convoy of fuel, ammunition and supplies. Just behind him, in another armored troop carrier, one of Medina's soldiers was videotaping. Suddenly, the screen shakes. Black smoke jets into the air. Noise, swearing, confusion erupts.
A roadside bomb had exploded directly beside Medina. Metal slag ripped through his vehicle's heavy armor, destroying radio equipment and blowing open Medina's door.
Outwardly, Medina did not appear seriously injured. But in the weeks and months that followed, his mind began to fail him. He slurred his words, then started stuttering. An avid reader, he struggled to get through a single page. A punctilious soldier, he began showing up late for missions.
Medina was sent to Germany in August, where Army doctors diagnosed him as suffering from a traumatic brain injury. But when he returned to Fort Bliss for treatment, he and his wife, Roxana, found themselves fighting for care.
Medina had his first appointment with Theeler a month after his return to Ft. Bliss. Afterwards, Theeler wrote that Medina had "multiple cognitive symptoms including poor concentration, short-term memory loss, and difficulty multi-tasking." Theeler said those symptoms were "possibly" related to lingering effects from his concussion, but were "likely" caused by "chronic headaches" and "anxiety." He wrote that Medina's stuttering was probably caused by anxiety, too.
After a follow-up session with Medina in December, Theeler wrote:, "I am concerned that he may be slipping into a cycle of playing the sick role." He pointed to the fact that Medina was using crutches -- apparently unaware that a physical therapist had asked Medina to use the crutches because of back pain.
To Medina, 34, a tall, broad-chested man with an intense stare, Theeler's words were insulting. Once praised by superiors for his leadership abilities, Medina worked relentlessly to overcome the staccato stutter that had made him difficult to understand. He was fighting to get better, fighting to remain in the Army. He said he felt he was being labeled a liar.
"You have all these values that you live for and fight for. And you go to the medical side and you don't see those values," Medina said. "I can understand being injured by insurgents. But I can't understand being injured by my own people."
Other soldiers had similar experiences with Theeler.
By the time Spec. Ron Kapture got to Fort Bliss in July 2009, he had suffered six concussions in which he was knocked unconscious from blasts, according to medical records and his own recollections.
He was suffering headaches on a daily basis. He noticed that he could no longer do simple mental tasks. Before joining the Army, Kapture had gone to vocational school to learn cabinet making. After returning from Iraq, he struggled to put together a bird house with his son.
"It took us about a month," said Kapture, 28. "I could build a whole living room full of furniture in a day seven years ago. It took me a month to build a bird house. That is frustrating stuff."
Five months after his return, Kapture finally got an appointment to see Theeler after making repeated requests. Theeler noted that Kapture had a history of "mild concussions," but blamed his cognitive problems on "chronic headaches, sleep disorder and underlying mood anxiety disorders and depressions," records show.
Kapture received counseling and medication for post-traumatic stress disorder, or PTSD, but his problems with memory and concentration persisted. He had planned to make the Army his career, but became so embittered at the handling of his care that he is applying for a medical dismissal.
"If that's the best help they ... can give us, then God help us all," Kapture said. "If that's the best they have to offer, I feel sorry for the guys coming home."
In an interview at the base, Theeler declined to comment on individual cases, even in cases where soldiers had signed a waiver of their privacy rights. He said, more generally, that he understood why soldiers like Medina and Kapture were frustrated. Mild traumatic brain injury can be difficult to pinpoint as a cause for soldiers' problems since there are no readily available biological markers to indicate that a concussion has occurred, he said.
Theeler said he concentrated on treating soldiers' symptoms regardless of the cause.
Soldiers "say, 'Sir, what's wrong with me?'" Theeler said. "We're honest. I say, 'I don't know what's wrong.' This is an area that we're working very hard at to get our hands around. I don't know the answers."
The PTSD Clinic
Some doctors and soldiers at Fort Bliss said medical commanders have placed a higher priority on treating post-traumatic stress disorder, a psychological condition, than on mild traumatic brain injury.
As evidence, they point to the fate of two clinics. While Building 805 remains unopened, the base has poured money and effort into an experimental PTSD clinic that has attracted widespread attention within the military, including a visit from Defense Secretary Robert Gates.
Known as the Restoration and Resilience Center, the clinic offers intensive, six-month-long treatment for chronic PTSD sufferers, including controversial techniques such as reiki, in which practitioners hover their hands over patients' bodies to improve the flow of "life energy," according to a pamphlet distributed at the center.
Brain injuries and PTSD sometimes share common symptoms and co-exist in soldiers, brought on by the same terrifying events. Neuropsychologists said that treatments for the conditions can differ, however. A typical PTSD program, for instance, doesn't provide cognitive rehabilitation therapy. Someone with nightmares associated with PTSD might be prescribed sleep medication, which could leave a brain-injured patient overly sedated without having a therapeutic effect.
One doctor at Ft. Bliss said that base commanders' focus on the PTSD clinic resulted in soldiers not getting adequate treatment for brain injuries.
"The way our philosophy is in this hospital ... we took away their belief that they truly have something," said the doctor, who did not want his name used for fear of retaliation from commanders. "I don't think we gave them the opportunity to heal and that's what I find really disgusting."
Some soldiers said they spent months receiving PTSD treatment while their cognitive problems went unaddressed.
Sgt. William Fraas, 38, the sergeant who was awarded the Bronze Star With Valor, served three tours in Iraq, helping to train the Iraqi soldiers as part of the 101st Airborne Division, 320th Field Artillery. He was given his medal after after rescuing an Army major and six Iraqi soldiers pinned down by gunfire. Driving in his Humvee, he used to keep track of the roadside bombs with a black grease pencil on the windshield. After 10, he stopped counting.
When he was sent home to Fort Bliss in 2008, he was diagnosed with PTSD and entered the experimental clinic. He spent eight months there before being cleared to return to active duty.
But Fraas realized he was still having problems. He was constantly dizzy. He had debilitating headaches. He would call his wife when driving, so she could keep him oriented and awake.
He began having blackouts. Once, he awoke to find his 12-year-old son struggling to lift him after he collapsed in front of his home computer.
"They have these meetings for PTSD. But nowhere did they tell you anything about TBIs. We had no idea what was going on," he said. "It feels like my head is loose. Like my brain is loose. Like it's rattling inside my head."
Finally, last summer, Fort Bliss doctors sent him to see a physical therapist at the base to improve his balance. But the appointments were irregular. And with his inability to drive, he had trouble getting around the sprawling base. A case manager who was supposed to coordinate his care asked one of Fraas' friends if he was faking it. A second case manager never even contacted him.
After putting nearly 20 years into the military, he was stunned.
"I could not get help. I called and called and called. I was hurting," he said. "It was just terrible. I'm a senior non-commissioned officer and I couldn't get help. I couldn't get help anywhere."
Mentis
Some Fort Bliss soldiers have discovered that if they protest long and loud enough about their care, base commanders occasionally will pay to send them for help -- outside the military.
On a hot afternoon earlier this spring, Sgt. Brandon Sanford was digging a small trench in the black soil of a rose garden at Mentis, a private neurological rehabilitation facility perched on the mountains just outside of El Paso.
He was installing an irrigation drip line as part of a therapy program designed to help him follow instructions. He set in one line, then covered up the trench. Then, looking down, he suddenly realized that he had failed to install the second drip line he was holding in his hand.
It was a typical problem for a brain-injury patient. Concentration deficits can make even simple tasks complex and confusing. Sanford immediately began pulling up the first line, digging again.
"That can be frustrating," the therapist overseeing the exercise said sympathetically.
"Never," said Sanford cheerfully. "I ate my Wheaties this morning."
Almost two years ago to the day, Sanford, a dog handler working with the 4th Infantry Division, was inside his Stryker troop carrier near Taji in central Iraq when a bomb exploded. The blast sent Sanford and his dog, Rexo, hurtling against the walls. Both were awarded the Purple Heart for shrapnel wounds they received in the explosion. Although dazed, Sanford shrugged off the headaches and dizziness he experienced and continued working.
When Sanford returned to Fort Bliss in January 2009, he began having seizures, along with continued headaches and balance problems. He saw the base neurologist, Theeler, who diagnosed him as having "shaking syndrome," medical records show.
He entered the PTSD clinic, received counseling and was released, but was still so mentally foggy he couldn't understand his 10-year-old son's math homework. His wife would open the cupboard where they kept cleaning supplies and find that her husband had put the milk carton next to the bleach. Sanford's wife and mother badgered military commanders unrelentingly until, nearly a year after his return from Iraq, they finally sent him to Mentis.
There, Sanford is an in-patient: he spends eight hours a day, five days a week, on rehabilitation exercises. He goes on weekly outings to help him navigate the noise and confusion of public spaces, such as shopping malls. And he practices real-world tasks, like following cooking recipes -- or laying out plans for a garden.
Today, Sanford said that he is able to finish making meals more quickly. He can now perform two tasks at once, instead of only one. He is getting better at managing his own medications and his balance has improved.
"You can only do so much sitting inside a hospital. It was like pulling teeth from a tiger to try to get in here. Once I got in here, it was like a whole new ray of light."
Eric Spier, Mentis' medical director, said he has asked the military to send him more patients. But base commanders have sent only a few dozen in almost three years.
"I've made sure to tell everyone I can tell that I'm ready to help, but that's all I can do," Spier said. The base has not sent "very many. It's surprisingly few."
Fraas and Medina now attend sessions at Mentis. They praised the facility, but expressed disappointment that they had had to go outside the Army to receive help.
Medina started in February. The staff at Mentis say his reading and concentration abilities are improving. His growing optimism is apparent in the blog he has started to chronicle his recovery.
"I might be slower right now, but I think it's all going to get better and I want to go back to what I love doing, which is soldiering," Medina said. "It's what I love to do."
Soldier Brain Injuries to Get Senate Scrutiny After ProPublica, NPR Report
"The recent NPR and ProPublica reports on the military's diagnosis, treatment, and tracking of traumatic brain injuries are concerning," Sen. Carl Levin, D-Mich., said in a statement.
NPR and ProPublica reported this week that the military was failing to diagnose soldiers with so-called mild traumatic brain injuries. Such injuries, also called concussions, are typically difficult to detect but can cause lasting mental and physical difficulties.
Unpublished military studies and interviews with medical officials suggest there could be tens of thousands of soldiers suffering undiagnosed traumatic brain injuries, which have been called one of the signature wounds in the wars in Iraq and Afghanistan. When soldiers were diagnosed, many received little or no treatment, even at large bases such as Fort Bliss in El Paso, Texas.
Official military statistics say 115,000 troops have suffered a mild traumatic brain injury since the wars began. But in interviews, top Army medical officials acknowledged that those figures understate the true number.
Civilian studies suggest up to 15 percent of people with mild traumatic brain injuries experience lingering problems with memory, concentration, sleep and balance problems.
"While the Department of Defense and the military services have made progress toward increasing knowledge about and awareness of the causes, diagnosis, and treatment of traumatic brain injuries, there is still a good deal to learn, both in the military and civilian medical environments," Levin said in his statement.
Levin2019s spokeswoman said the hearing will take place later this month, though the date has not been finalized. It will look at the complex web of illnesses that have afflicted troops returning from the wars in Iraq and Afghanistan and the role those disorders play in soldier suicides. The issue has been a growing concern in the military.
Soldiers with traumatic brain injury often also suffer from post-traumatic stress disorder, or PTSD, a debilitating psychological wound. Those who survive roadside blasts can suffer both a brain injury and PTSD, which can be triggered by the terror of the event.
"Traumatic brain injury, post traumatic stress, and suicide are all related issues, at times making diagnosis difficult," Levin said in his statement.
Army officials said they have been working to improve their systems to diagnose soldiers. They said soldiers with brain injuries have received appropriate treatment.
In an interview earlier this week, Gen. Peter Chiarelli, the Army's vice chief of staff, said the military took traumatic brain injuries "extremely seriously."
Chiarelli, who has worked to raise awareness about the severity of so-called invisible wounds such as mild traumatic brain injury and PTSD, said medical officials must diagnose and treat a complicated mix of illnesses.
"It's time we realize that TBI and PTSD are real injuries," Chiarelli told "Talk of the Nation" host Neal Conan. "We've got to ensure our soldiers get the care that they need."
Congress Demands Answers on Brain Injury Care at Texas Base
Rep. Harry Teague, D-N.M., Rep. Silvestre Reyes, D-Texas, and Rep. Ciro Rodriguez, D-Texas, sent a letter to Fort Bliss' William Beaumont Army Medical Center on Tuesday expressing concern over our report that soldiers encountered debilitating delays and frustrating bureaucracy when seeking help at the base, America's third largest by number of soldiers.
A spokeswoman for Teague said today that the congressman was also considering calling for the U.S. Government Accountability Office to review the military's handling of traumatic brain injuries and may pay a visit to Fort Bliss to personally inspect the facilities.
"We are deeply concerned that our government could be failing those to whom we owe the most," the three men wrote in their letter. "These reports must be investigated and receive the full attention of the United States Congress and government."
In our investigation, we found that soldiers at Fort Bliss struggled to receive diagnosis and treatment for so-called mild traumatic brain injury. Such head traumas, also called concussions, often leave no visible signs of damage, but can result in long-term mental and physical problems.
Official military figures show that about 115,000 troops have suffered mild traumatic brain injuries since 2002. But we found that many troops have injuries that go undiagnosed or that are never documented in their medical records. Top Pentagon officials acknowledged in interviews that the true toll is likely far higher. Unpublished military studies reviewed by ProPublica and NPR suggest tens of thousands of mild traumatic brain injuries have gone uncounted.
Most soldiers with concussions recover quickly, but civilian studies indicate that 5 percent to 15 percent of those who suffer such injuries have lingering cognitive problems.
The Senate Armed Services Committee announced Wednesday that it will hold a hearing on June 22 to look into suicide, traumatic brain injury and other so-called invisible wounds.
Our investigation found that Fort Bliss had erected billions of dollars of new housing and accommodations for additional troops to deploy to war zones, but had failed to open the doors of Building 805, a traumatic brain injury clinic completed nearly a year ago. Although the Pentagon designated the base as a site for enhanced treatment for brain-injured soldiers in 2007, the base did not hire a full-time director for the program until October 2009.
Soldiers at Fort Bliss told us they waited weeks or months just to get appointments to see doctors and often received far fewer hours of therapy than patients at well-regarded civilian clinics. Some were prescribed therapy for psychological problems that did little to relieve their troubles with memory, balance and reasoning.
The three congressmen, who are part of the bipartisan Congressional Invisible Wounds Caucus, have asked the medical commander at Fort Bliss, Col. James Baunchalk, to answer several questions about the base hospital's treatment program.
They asked to know how many patients with traumatic brain injury, or TBI, were being treated at Fort Bliss, how long soldiers had to wait for appointments, and whether the hospital had systems in place to address soldiers' complaints.
"It's pretty important that (Fort Bliss) be at the front of addressing TBI and PTSD," Teague said in an interview. PTSD, or post-traumatic stress disorder, is a psychological wound that often accompanies TBI.
Fort Bliss officials have declined to answer such questions from ProPublica and NPR. Baunchalk also denied ever having received complaints regarding brain injury care, despite e-mails and letters written to his assistants and superiors by soldiers and family members.
Fort Bliss officials have defended their treatment of soldiers. In a response this evening, a base spokesman said they would respond to all questions posed by the congressmen by June 21.
"Our commitment is to provide quality health care, in a timely manner, to those who serve in our military," the statement said.
Congress Questions Military Leaders on Suicides, Traumatic Brain Injury
Responding to what he called "disconcerting" reports by NPR and ProPublica, Sen. Carl Levin, D-Mich., said at a hearing before the Senate Armed Services Committee that the military needed to better address the wide range of medical and behavioral problems affecting troops.
Earlier this month, we reported that the military was failing to diagnose and adequately treat troops with brain injuries. Since 2002, official military figures show more than 115,000 soldiers have suffered mild traumatic brain injuries, also called concussions, which leave no visible scars but can cause lasting problems with memory, concentration and other cognitive functions.
But the unpublished studies that we obtained and the experts that we talked to said that military screens were missing tens of thousands of additional cases. We also talked to soldiers at one of the military's largest bases, who complained of trouble getting treatment.
"I am greatly concerned about the increasing number of troops returning from combat with post-traumatic stress and traumatic brain injuries, and the number of those troops who may have experienced concussive injuries that were never diagnosed," Levin, chairman of the committee, said as he opened today's hearing.
Gen. Peter Chiarelli, the Army's vice chief of staff, said the Army had made strides in identifying soldiers at risk of committing suicide, setting up new treatment centers and deploying a new system of "telemental health services," allowing soldiers to talk with counselors by computer video chat programs.
Chiarelli's remarks were echoed by other senior military commanders at the hearing from the Navy, Air Force and Marine Corps.
"Our success notwithstanding, we still have much more to do," said Chiarelli, who has emerged as the Army's point man on mental health issues. "We face an Army-wide problem that will be only be solved by the coordinated efforts of our commanders, leaders, soldiers and program managers and health providers. This is a holistic problem with holistic solutions and that is how we're approaching it."
Chiarelli acknowledged that the Army continues to have problems with properly diagnosing soldiers with mild traumatic brain injuries, saying that it was an emerging area of medicine. And he acknowledged that soldiers at bases throughout the Army have sometimes had trouble receiving treatment for mild traumatic brain injuries and post-traumatic stress.
Chiarelli took issue with our reporting, however. He said the NPR and ProPublica reports were wrong to blame military doctors for failing to diagnose the problem, or to accuse senior military officials of not taking the issue seriously. He also said that NPR and ProPublica had tried to draw a distinction between traumatic brain injury, or TBI, and post-traumatic stress, or PTS, two conditions which frequently occur together.
"I think the great disservice that NPR did to everyone was to try to isolate TBI from PTS. And that is just not possible," Chiarelli said. "The co-morbidity of these two is what's giving us the difficulty today. And I also think that they did a disservice when they indicated that PTS is a psychological problem. It's not just at a psychological problem. It is a physical injury that occurs."
Chiarelli did not cite any factual errors in the stories and we stand by our reporting. But we also think he is mischaracterizing our reporting, which was based on dozens of interviews with senior military researchers, commanders and soldiers, and thousands of pages of unpublished studies, e-mails and medical records.
First, we did address the overlap of TBI and PTSD in our stories: "To be sure, brain injuries and PTSD sometimes share common symptoms and co-exist in soldiers, brought on by the same terrifying events," we wrote.
We also did not downplay the seriousness of PTSD -- a wound which NPR has reported on extensively in past stories.
We found several instances in which military doctors expressed skepticism about mild traumatic brain injury and its effects. Dr. Charles Hoge, one of the Army's senior health advisers, referred to the "illusory demands" of mild traumatic brain injury in an opinion piece in the New England Journal of Medicine last year. In an April 2010 e-mail that we obtained, he wrote: "What's the harm in missing the diagnosis of mild TBI?" In an interview, Hoge told us that he was concerned with treating soldiers' symptoms, no matter the cause.
We also turned up extensive evidence that military doctors weren't diagnosing mild traumatic brain injuries, both on the battlefield and when troops came home. Battlefield medics, overwhelmed by life-threatening wounds, can miss the signs of concussions. Screening tools now in place often fail to catch soldiers who have suffered concussions. Soldiers often try to hide their symptoms to return to battle with their comrades.
One of the Army's senior neuropsychologists told us of examining five soldiers who had survived a rocket attack in Iraq last year. Medical staff had treated their visible wounds, but failed to diagnose them as suffering from mild traumatic brain injury -- even though they were suffering "classic" symptoms, according to Lt. Col. Mike Russell.
It is important to diagnose mild traumatic brain injury and quickly provide treatment for any lingering effects, according to the Pentagon's own experts. While the majority of soldiers recover quickly from concussions, some report lasting mental and physical problems. Studies show that such soldiers can be helped by providing cognitive rehabilitative therapy, an intensive program to retrain the brain to perform mental tasks.
Sen. Mark Udall, D-Colo., asked Chiarelli several questions about the military's efforts to improve how it diagnoses traumatic brain injury. Afterwards, he said that he appreciated Chiarelli's efforts, but planned to continue pressing Army officials on the issue.
Udall "remains concerned about the impact of TBI and PTSD on our service members," Tara Trujillo, a Udall spokeswoman. "As discussed at the hearing, there is much still to learn, different approaches to take and ways to continue to improve."
After the hearing, Levin said he was convinced that the services were trying to properly diagnose mild traumatic brain injury.
"I remain concerned about the diagnosis of traumatic brain injuries, and especially of mild traumatic brain injuries, but it is not for lack of the services trying to do the best they can with existing science, tools, and methods," Levin said in a statement. "There is still much to be learned in both the military and civilian medical environments about the diagnosis, treatment, and care of traumatic brain injury, and its relationship to other combat-related injuries such as post traumatic stress. I believe each of the services is taking the issues of detection, tracking, and follow-up care very seriously, but there is still work to be done."
Leader of Military’s Program to Treat Brain Injuries Steps Down Abruptly
WASHINGTON, D.C.--The leader of the Pentagon's premier program for treatment and research into brain injury and post traumatic stress disorders has unexpectedly stepped down from her post, according to senior medical and congressional officials.
Brig. Gen. Loree Sutton told staff members at the Defense Centers of Excellence, or DCOE, on Monday that she was giving up her position as director. Sutton, who launched the center in November 2007, had been expected to retire next year, officials with knowledge of the situation said. The center has not publicly announced her leaving.
Sutton's departure follows criticism in Congress over the performance of the center and in recent reports by NPR and ProPublica that the military is failing to diagnose and treat soldiers suffering from so-called mild traumatic brain injuries, also called concussions.
It comes just as the Pentagon prepares to open a new, multimillion-dollar showcase treatment facility outside Washington, D.C., for troops with brain injuries and post traumatic stress disorder, often referred to as the signature wounds of the wars in Iraq and Afghanistan.
Late Wednesday, in a sign of disarray within the program, Sutton cancelled a scheduled appearance at the opening of the National Intrepid Center of Excellence, a gleaming new facility of waving glass and futuristic virtual reality treatment rooms in Bethesda.
"The war in Iraq and Afghanistan could end tomorrow; our mission to restore health, hope and humanity will endure for decades," Sutton wrote in her farewell message. "We simply must uphold our commitment to all who have borne the burdens of war on our behalf."
Sutton did not respond to requests for comment. Her replacement, U.S. Army Col. Bob Saum, also declined to comment.
Cathy Haight, the acting spokeswoman for DCOE, said Sutton's departure, though apparently well ahead of schedule, was part of a routine command rotation. Haight said Sutton decided to leave after turning down the Army's offer to take a new position overseeing the military medical system in Europe.
"If a general officer declines (a new position)...they are in a transition to retire," Haight said.
In recent months, legislators have questioned Sutton's ability to carry out the mission of the centers, which is to catalyze research and treatment across the military for soldiers returning with brain injuries and psychological wounds.
Congress directed the military in 2008 to create the brain injury center and other facilities for wounded soldiers. At an April hearing of a House Armed Services subcommittee, Rep. Susan Davis, D-Calif., said that the center had failed to carry out its role.
"The Defense Center of Excellence, while having achieved some notable small scale successes, has not inspired great confidence or enthusiasm thus far. The great hope that it would serve as an information clearinghouse has not yet materialized," Davis said.
"The center has also made some serious management missteps that call into question its ability to properly administer such a large and important function," Davis continued.
Scrutiny of Sutton rose another notch earlier this month, when NPR and ProPublica reported on the military's problems in handling soldiers with mild traumatic brain injuries. Such injuries leave no visible scars, but can cause lasting mental and physical difficulties.
Military statistics show that about 115,000 troops have suffered such injuries since 2002, but in interviews, Army experts acknowledged the true toll may be far higher. Unpublished research we reviewed suggests that tens of thousands of soldiers may have gone undiagnosed. Our reporting also showed that even when soldiers were diagnosed, at one of America's largest Army bases, they have had to fight to receive appropriate treatment.
Still, some veterans' advocates were shocked and saddened that Sutton was leaving. They said she had been a forceful, visible advocate for wounded troops and their families who had never received the full support of the military's medical establishment.
Critics of the military's health system have noted a power vaccum at the top of the military medical structure. Four people in just over three years have rotated through the Pentagon's top health policy position, the assistant secretary of defense for health affairs.
"She was always there for the troops," said one veterans' advocate, who did not want to be named for fear of criticizing the military. "She's become the scapegoat."
In an April interview with NPR and ProPublica, Sutton shrugged off the criticism. "Leading change," she said, "is a journey not for the faint of heart."
"We are very proud of the team that we have built, the concept in terms of the center of centers, the network of networks," she said. "Are we anywhere close to where we want and need to be? No. Of course not."
Pentagon Shifts Its Story About Departure of Leader of Brain Injury Center
Earlier this month, we reported that the military was routinely failing to diagnose such injuries, which are the most common head wounds sustained by soldiers in Iraq and Afghanistan. We also found that soldiers had trouble getting adequate treatment at one of America's largest military bases, Fort Bliss in El Paso, Texas.
Since then, Congress and the military have taken a number of steps to redress the issues we raised. The Senate Armed Services, for instance, grilled military leaders on the topic at hearing. Rep. Harry Teague, D-N.M., wrote a letter demanding answers on the care at Fort Bliss.
We also reported last week that the leader of the Pentagon's premier research center into brain injury had unexpectedly stepped down just days before the June 24 dedication of a new, cutting-edge medical center for head traumas, post-traumatic stress disorder and other so-called invisible wounds of the wars in Iraq and Afghanistan.
Then things got strange. Our story quoted a spokeswoman for Brig. Gen. Loree Sutton who said Sutton was stepping down from the Defense Centers of Excellence because she had turned down a post in the military's European medical command, a decision that meant she would retire. The spokeswoman, Cathy Haight, described it as part of a normal process of command rotation.
Two days later, we got a message from Sutton's boss, Charles Rice, the assistant secretary of defense for health affairs. A Pentagon spokeswoman, Eileen Lainez, said that Haight "misspoke." Sutton stepped down after Rice decided "that a change in leadership was necessary to continue moving the organization forward," Lainez said.
This struck us as odd. Was Rice going out of his way to tell us that he had fired Sutton? If so, why? And why did he decide to ask Sutton to step down only days before the dedication of the National Intrepid Center of Excellence?
Lainez had no further comment. "I'm just providing clarification on the reassignment," she said.
Then it got weirder still. As part of the original story, which ran the day before the dedication, we reported that Sutton had canceled her appearance at the ceremony, citing this press release from the center: "BG Loree K. Sutton will no longer be in attendance."
Afterward, another spokeswoman for the general contacted us to say that Sutton had never canceled. She said the press release issued by the center was wrong. Sutton had attended the ceremony and several related events.
"Clearly, there was some confusion and I understand how this mistake could occur in the final hours of preparation of the event," Judith Evans wrote. Sutton, she said, "was seated in a VIP section ... and acknowledged by speakers during remarks at the ceremony."
Evans declined to answer any follow-up questions on Sutton, who also did not respond to requests for clarification. The Defense Centers of Excellence still has not announced her departure publicly. Sutton now works in the office of Army Surgeon General Eric Schoomaker.
The new center, which is in Bethesda, Md., apologized for the error: "We understood the information about Gen. Sutton's attendance at the NICoE dedication ceremony to be correct at the time and regret any miscommunication," said Jody Fisher, a spokesman for Rubenstein Communications, the firm that handled PR for the event. "We were very pleased that she was able to attend the event."
Sutton had both fans and enemies, as we reported. Congress found fault with her management skills, but some veterans' advocates praised her tireless devotion to soldiers and their families.
Critics of the military's health system have noted a power vacuum at the top of the military medical structure. Four people in just over three years have rotated through the Pentagon's top health position, the assistant secretary of defense for health affairs.
One figure reportedly upset by the way the new $65 million brain-injury center debuted was Arnold Fisher, a New York real estate magnate and philanthropist who led the fundraising to build it.
Fisher, according to The Washington Post, said it was "unacceptable" to ignore the needs of wounded veterans. He criticized the White House for not sending any representatives to the ceremony.
"These are the very people who decide your fate," Fisher told the Post. "We are all here, but where are they?"
Fort Bliss Says It Will Examine Its Handling of Brain Injuries
Medical commanders at one of America's largest military bases have ordered a review into the care provided to soldiers suffering from traumatic brain injury, in response to an investigation by NPR and ProPublica.
Col. James Baunchalk, the commander of William Beaumont Army Medical Center at Fort Bliss in El Paso, Texas, told members of Congress that he was concerned by our report, which found that soldiers there struggled to receive adequate care for mild traumatic brain injuries.
The hospital is "committed to delivering the very highest quality care and support to our soldiers and their families, including those who may be affected by traumatic brain injuries," Baunchalk wrote in a June 21 letter to Rep. Harry Teague, D-N.M., a copy of which was obtained by NPR and ProPublica.
The Pentagon's official figures show that more than 115,000 troops have suffered mild traumatic brain injuries, also called concussions, since the wars began in Iraq and Afghanistan. But our story said those figures likely understate the true toll, with some studies suggesting that the injuries go undiagnosed in tens of thousands of troops. While most recover quickly, some grapple with lasting mental and physical problems from exposure to explosions.
Our story focused on several soldiers at Fort Bliss, the third-largest American military base by troop population. The soldiers told us they endured long waits to see specialists and met with frustrating skepticism from doctors over the severity of their conditions. All had ongoing problems with memory, concentration and other cognitive functions.
We also wrote about Building 805, a small clinic at the base that was supposed to screen soldiers with traumatic brain injuries. Although the base has recently added billions of dollars of barracks and other facilities to accommodate newly arriving troops, Building 805 has remained shuttered for almost a year, for want of computer wiring, commanders told us.
Teague, who visited the base on Sunday and met with soldiers mentioned in our story, said he would continue to press the hospital to make sure that adequate care was being delivered.
"I would like to further examine how the overall quality of TBI care at Fort Bliss serves our soldiers compared to what they may have access to in civilian medicine," Teague wrote in a June 25 letter to Baunchalk. "I would like to ensure that the system of TBI care, in general, adequately addresses the needs of our service members and is adequately resourced."
Base officials did not immediately respond to requests for comment on their letter to Teague. The letter listed a series of programs in place to treat soldiers and catch problems in care, but some of the information appeared to contradict material that base officials provided to us.
Fort Bliss told Teague it had 10 medical staff members "assigned full time" to the traumatic brain injury program. But in a letter responding to our questions in April, officials listed only four employees providing such care full-time. They listed seven other clinicians who worked part-time with brain-injured patients.
Fort Bliss also told Teague that Building 805 was "completed at the end of January 2010." But in interviews with us and in their written response to our questions, base officials told us that Building 805 "was completed in July 2009," though utilities were not installed until February 2010.
Fort Bliss officials also told us during our visit there in April that Building 805 would be open at the end of May. In their letter to Teague, they said that they had not even issued a contract to install the computer wiring until June 17 2014 nine days after our stories ran.
Sgt. Victor Medina and his wife, Roxana Delgado, who were featured in our stories, said they were pleased that Teague and others have paid attention to soldiers' concerns about treatment for brain injuries. Medina had to fight to get referred off base to a private medical facility specializing in cognitive rehabilitation.
But, they said, more work remains to be done.
"We're seeing a lot of progress in terms of attention and interest," Delgado said. "But we want to see more. We want to see real reform."
Update: Fort Bliss got back to us on Thursday to respond to our questions with this letter. They reiterated that the Fort Bliss program has 10 "full time" clinicians devoted to traumatic brain injury, though one slot is vacant.
They also said that Building 805, a clinic for screening soldiers with traumatic brain injury, was completed for occupancy earlier this week. The process to move in clinical staff has begun, according to the written responses.
Finally, Fort Bliss acknowledged for the first time that the base has not yet received full validation under Defense Department guidelines for its traumatic brain injury treatment program. Fort Bliss is designated a "Level 2" facility, meaning it is supposed to have one of the top 10 treatment programs in the U.S. to address mild and moderate brain damage. Fort Bliss officials said Thursday that the base passed an initial round of examination, but does not expect to receive full validation of its program until Fall 2010.
Rep. Teague Pledges Deeper Inquiry Into Treatment for Brain-Injured Soldiers
In a letter to medical commanders at Fort Bliss, the third-largest Army base in the country, Teague, D-N.M., wrote that he had turned up troubling evidence of systemic problems across the military in the treatment of soldiers suffering lingering cognitive difficulties as a result of roadside blasts.
Teague launched his inquiry after an investigation in June by NPR and ProPublica found that the military's medical system had failed to diagnose and treat tens of thousands of soldiers that had suffered mild traumatic brain injuries, often called one of the wars' signature injuries. The reports also found that soldiers had to fight for treatment at the military hospital at Fort Bliss, a base in El Paso, Texas that sprawls into Teague's district.
Teague said he planned to ask the Government Accountability Office, Congress' investigative arm, to conduct a "comprehensive examination" of the care provided to soldiers with traumatic brain injuries in the Defense Department and Veterans Affairs' medical systems.
"I am concerned that Fort Bliss, and by extension the military, is not adequately identifying, assessing, and treating patients with mild to moderate TBI case," Teague wrote.
A spokeswoman for the Pentagon said today that they were reviewing the letter. A Fort Bliss hospital spokesman said base commanders have not yet had time to respond to Teague's concerns.
The hospital's former commander had promised a "thorough review" of the care and treatment of soldiers after the NPR and ProPublica stories. A Fort Bliss spokesman said Friday he does not know if the review has been conducted.
Official military figures show that about 115,000 troops have suffered mild traumatic brain injuries since 2002. But based on interviews and unpublished military studies, we found evidence suggesting that tens of thousands go undiagnosed or sustain injuries that are never documented. Mild traumatic brain injuries, also known as concussions, are often referred to as invisible wounds because they are difficult to detect and leave no visible scars.
While most soldiers with concussions recover, civilian studies indicate that between 5 percent and 15 percent of people who suffer mild traumatic brain injuries have lingering cognitive problems. Unpublished studies of soldiers echo those findings. Such soldiers have trouble remembering, following directions or doing more than one task at a time.
Teague said that he had several concerns about the state of care at Fort Bliss. He said his investigators found that the Fort Bliss program had not been accredited by the Commission on the Accreditation of Rehabilitation Facilities, a leading trade organization.
He also said he was concerned that Fort Bliss did not have enough staff to treat the more than 1,100 soldiers who were diagnosed on base last year as suffering continuing problems from mild traumatic brain injuries. All in all, Teague wrote, soldiers with mild traumatic brain injuries were not receiving a high level of medical care.
He said that Fort Bliss and the military medical system needed to develop a comprehensive system of rehabilitation to help soldiers with continuing problems as a result of sustaining concussions.
"Our response to the epidemic of TBI among our service members and veterans should be overwhelming and unambiguous," he wrote. "The U.S. government should marshal every resource to treat and heal the invisible wounds of our current wars in Iraq and Afghanistan."
Fact Sheet: Traumatic Brain Injury
What is it? And how does it differ from a concussion?
Traumatic brain injury, or TBI, is a sudden trauma to the brain caused by force. A severe TBI can leave a person almost incapable of functioning. But even a mild TBI -- a concussion -- can lead to a range of debilitating symptoms: headaches, balance problems, hearing problems, lack of self-control, mood changes, ringing in the ears, problems sleeping and memory loss. While most people recover from a mild TBI, it can take months, even years.
According to the Centers for Disease Control and Prevention, "approximately 1.7 million people sustain a traumatic brain injury annually" in the United States, and "the majority of TBIs each year are concussions or other forms of mild TBI." For some basics on the science behind TBIs, see NOVA Science Now's "Brain Trauma" video and website.
The brain injuries sustained by soldiers serving in Iraq and Afghanistan are most often caused by explosives. See ProPublica's graphic showing what happens to the brain during and after a blast.
How many U.S. soldiers have TBI?
The exact number is hard to pinpoint. The Pentagon says about 115,000 soldiers have mild TBI, while the RAND Corporation study Invisible Wounds of War suggests the much higher number of 400,000 total TBIs, the majority of which are mild.
How is TBI diagnosed?
Diagnosing TBI can be hard. Symptoms of moderate to severe TBI can be obvious -- extended loss of consciousness and severe neurological disorders -- but diagnosing a mild TBI is trickier, especially during combat. Often soldiers don't even realize they have a mild brain injury after a blast. In some cases, combat medical records are lost or destroyed in theater.
And NPR and ProPublica found that "the military's doctors and screening systems routinely miss brain trauma in soldiers."
The military uses two basic tests to diagnose the injury: The first, the Military Acute Concussion Evaluation, or MACE, is a survey taken immediately after an injury. NPR and ProPublica found that often soldiers learn to cheat on this test because they want to return to their platoon. The second, Automated Neuropsychological Assessment Metrics, or ANAM, "failed to catch nearly half of all soldiers who had suffered a concussion, according to a recent unpublished study obtained by NPR and ProPublica. Lt. Gen. Eric Scoomaker, the Army's top medical official, recently testified in Congress that results from the test are no better than a 'coin flip.'"
Another consideration in diagnosing TBI is its comorbidity with PTSD. In a response to NPR and ProPublica, Gen. Peter W. Chiarelli, the Army vice chief of staff, said "it was a mistake to focus solely on TBIs, since many soldiers are also suffering from post-traumatic stress, or PTS[D], a debilitating psychological wound that can be caused by the intense terror of being involved in a roadside blast. ...He said the military was diagnosing and treating soldiers suffering from both wounds."
(See a timeline tracking the effort to diagnose and treat TBI.)
How is TBI treated?
Treatment varies widely. There's no standard treatment. Although NPR and ProPublica found that regular and consistent cognitive rehabilitation therapy -- techniques to compensate for decreases in mental function -- benefited several veterans, this type of treatment is rarely available through military medical care. Many soldiers have sought rehabilitative treatment at private facilities. For each of the three soldiers profiled in FRONTLINE's The Wounded Platoon the most common treatment given for their diagnosed TBI was pharmacological.
There is some hope that treatment in hyperbaric oxygen chambers might aid in recovery. A study on this therapy gets underway in 2011 and will be conducted at five U.S. bases by the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
The most common way to prevent chronic TBI is to rest after receiving an injury to the head. The Pentagon recently released a new policy for the treatment of TBI, which includes a mandatory 24-hour rest period after a blast, and a complete neurological assessment for soldiers who have had three concussions. If a soldier with TBI is not taken out of theater to properly recover, any additional brain injuries can exacerbate the damage. Yet, as noted above, some soldiers may not realize they have TBI, or they brush off symptoms in order to rejoin their platoon.
Soldiers With Brain Trauma Denied Purple Hearts, Adding Insult to Injury
A version of this story was aired on NPR's "All Things Considered." Listen to the audio of that broadcast below:
The U.S. Army honors soldiers wounded or killed in combat with the Purple Heart, a powerful symbol designed to recognize their sacrifice and service.
Yet Army commanders have routinely denied Purple Hearts to soldiers who have sustained concussions in Iraq, despite regulations that make such wounds eligible for the medal, an investigation by NPR and ProPublica has found.
Soldiers have had to battle for months and sometimes years to prove that these wounds, also called mild traumatic brain injuries, merit the honor, our reporting showed. Commanders turned down some soldiers despite well-documented blast wounds that wrenched their minds, altered their lives and wracked their families.
The Army twice denied a Purple Heart for Sgt. Nathan Scheller, though the aftereffects from two roadside explosions in Iraq have left him with lasting cognitive problems, according to the Army's own records.
The 29-year-old former tank commander navigated an M1A1 Abrams through Baghdad's urban battlefield of bomb strewn highways and sniper filled alleys. Now he gets lost driving familiar routes around his home. An honor student in high school, he can no longer concentrate enough to read the adventure novels he once loved.
"I don't see how somebody else can tell me that I don't deserve one," Scheller said of the Purple Heart. "I may not have wounds on the outside. But I have wounds on the inside."
The denials of Purple Hearts reflect a broader skepticism within the military over the severity of mild traumatic brain injury, often described as one of the signature wounds of the conflicts, according to interviews, documents and internal e-mails obtained by NPR and ProPublica.
High level medical officials in the Army debated whether head traumas that are difficult to detect, often leaving no visible signs of damage, warrant the award, the e-mails show. Most people who sustain such blows, also known as concussions, recover on their own, but studies show 5 percent to 15 percent may have long-term impairments.
In 2008, Brig. Gen. Joseph Caravalho, then the top medical commander in Iraq, issued a policy blocking medical providers from even discussing the Purple Heart with soldiers who suffered mild traumatic brain injuries.
"In many cases," Caravalho wrote that concussions with "minimum medical intervention will not warrant this award."
His policy appears to contradict Army rules governing the Purple Heart.
Army regulations say that a soldier is entitled to the Purple Heart if injured by hostile action. The soldier must require treatment -- no matter how minimal -- by a medical officer, and the injury must be documented. Medical officers can offer advice on whether an injury merits recognition. The soldiers' commanding general typically makes the final decision to award or deny a Purple Heart.
The Army's official list of wounds that "clearly justify" the award includes, "Concussion injuries caused as a result of enemy generated explosions."
In an e-mailed response, Caravalho, who now commands one of the Army's top hospitals, said he was trying to help medical personnel understand some of the complexities involved in the diagnosis and treatment of mild traumatic brain injuries. He did not specifically address whether his order created new restrictions on the award of the medal.
"I was trying to make the point that medical providers in the field needed to ensure they documented the event, the findings and the treatment rendered," wrote Caravalho. "Without this corroborating documentation, I felt it would be increasingly difficult to support a Purple Heart request based solely on subjective, and potentially temporary symptoms."
Gen. Peter Chiarelli, the Army's second in command, said it is "very, very clear" that soldiers who have sustained documented concussions from enemy action should receive the Purple Heart. He said he was not aware of Caravalho's order until NPR and ProPublica brought it to his attention.
"This is a good catch," he said, saying he had asked Army lawyers to review the policy to see whether it should be changed. A Chiarelli spokesman said Wednesday that, as of last week, the review was continuing.
Chiarelli, the Army's point man on the treatment of traumatic brain injury and post traumatic stress, acknowledged there is ongoing resistance to awarding the Purple Heart for so-called "invisible" wounds.
He saw it firsthand when he served as commander in Baghdad from 2004 to 2005 and said he overturned many denials for the medal stemming from concussion injuries. There has been progress since then, he said, but more work remains.
"There still are some commanders, okay, who -- and there may be some doctors, too -- who don't feel that a concussion should entitle somebody for a Purple Heart," Chiarelli said. "But we have far more commanders that understand that the concussion is a real injury today than we had in 2004 and 2005."
"We are moving in the right direction to fix this."
A Certain Level of Tough
Created by George Washington in 1782 and revived 150 years later by Gen. Douglas MacArthur, the Purple Heart carries extraordinary significance.
Unique among military honors, it is an entitlement earned by all soldiers who meet the basic criteria. It does not depend upon a recommendation from a superior officer.
The Purple Heart confers practical benefits, gaining recipients a higher priority in obtaining medical service from Veterans Affairs medical facilities.
But for many soldiers, the Purple Heart is, first and foremost, a badge of courage: A tangible recognition of service, honor, and bravery.
Nearly 25,000 soldiers have been awarded Purple Hearts for all types of wounds suffered in Iraq and Afghanistan, according to the Army's Human Resources Command. A spokesman said the military does not know how many soldiers have received the Purple Heart for mild traumatic brain injuries, or how many have been denied. He said the Army doesn't keep track.
The number of Purple Hearts awarded is dwarfed by the number of soldiers who have suffered concussions. Official figures show about 90,000 Army soldiers have sustained mild traumatic brain injuries since 2002 -- though all those soldiers likely do no meet the criteria for the award. Tens of thousands of additional troops have gone undiagnosed, NPR and ProPublica reported in June, based on unpublished military studies, internal e-mails and interviews.
Some soldiers who have suffered mild traumatic brain injuries have received Purple Hearts. Sgt. Victor Medina, who was profiled in a previous story by NPR and ProPublica, received his award after his wife wrote to his commander insisting that he deserved the recognition.
"It would have been easier to get one if I had lost an arm or a leg. Then they could have seen it," Medina said.
The military's regulations to document the wound and treatment can make it difficult for someone with a mild traumatic brain injury to prove that the award criteria are met. Treatment for a head injury in the immediate aftermath of combat can be as little as bed rest, or pain medications which are not always noted in medical records.
Once they return home, some soldiers don't realize they have problems until months or years after the injury -- making it difficult to prove a link between the blast and their symptoms.
Sgts. James Hopkins and Derrick Junge are among those who have been diagnosed with concussions, but were passed over for the Purple Heart.
Hopkins and Junge suffered their injuries in January 2009 when a rocket slammed into a wall near their trailer at Camp Liberty in Baghdad. At the time, a senior Army neuropsychologist, Lt. Col. Mike Russell, was conducting a study on concussions. He diagnosed the men and three fellow soldiers as having suffered mild traumatic brain injuries during the attack, according to medical records.
Yet only one soldier in the trailer, who suffered shrapnel wounds in the attack, received the medal. The other men have been turned down by senior commanders.
Hopkins received a form letter telling him that his documentation was not sufficient. The letter did not tell him what documents he was missing or exactly why he was denied.
"I'm over there. I'm doing what I'm supposed to do. I'm giving everything that I'm supposed to," said Hopkins. "But I feel I'm not getting that same thing in return." Hopkins had splitting headaches and trouble walking for days after the explosion. He still forgets details today. He repeats himself in conversation, forgetting what he told his wife moments ago. Not getting a Purple Heart, he said, "That's a big slap in the face."
Like many soldiers who suffered a concussion, Junge has trouble remembering details of what happened after the explosion. He believes a medic might have given him headache medication, but has no documentation of the treatment.
Nor has Junge received rehabilitation or other treatment for ongoing mental difficulties. A former B-2 bomber mechanic, he sometimes struggles with simple tasks, such as building a tree house for his kids. He gets irritated easily. He forgets details and the names of common household items.
Junge said he didn't see a doctor because he wanted to keep leading his unit.
"As a soldier, you're expected to be a certain level of tough. It's across the board from top to bottom. If it's not a visible injury, it's kind of looked as a non-injury," he said. "For soldiers, it's like, are you a puss?"
For the families of soldiers with mild traumatic brain injuries, the Purple Heart is sometimes the only outward sign of the serious internal trauma endured by their loved ones.
"He thinks nothing is wrong. And it's like, I'm married to a totally different person," said Holly Junge, Derrick's wife, breaking down in tears as she spoke. "That's scary."
Junge is scheduled to deploy back to Afghanistan later this month.
If You're Not Bleeding, It's Not Serious
Congress, the military and veterans groups have wrestled for decades over how to define which injuries are worthy of the Purple Heart.
After the 1989 invasion of Panama, a debate erupted when a soldier received the medal for heat stroke. Two years ago, an Army psychologist raised a furor by suggesting that the Purple Heart should be given to soldiers suffering from post traumatic stress disorder, or PTSD.
The Pentagon specifically banned giving the award for the disorder, saying that PTSD is a secondary effect not directly caused by the enemy. The decision remains controversial.
Mild traumatic brain injuries, however, are not supposed to be part of the debate. For at least 50 years, military regulations have recognized concussions as an injury meriting the Purple Heart.
But now, in wars in which roadside bombs are the enemy's best weapon and with tens of thousands of soldiers suffering mild traumatic brain injuries, some military officials argue that giving the Purple Heart for concussions would lessen its value, according to sources and internal documents reviewed by NPR and ProPublica.
Mild traumatic brain injuries have become more common in Iraq and Afghanistan because of insurgents' heavy use of explosive devices and armor which has better protected soldiers from life-threatening injuries.
In late 2007, Col. Edward Neely, an Army neurologist then serving in Iraq, sent an impassioned e-mail to a group of fellow medical officers with the subject line "More Purple Hearts for Those Who Deserve It."
Neely said some senior medical officials opposed giving out the Purple Heart for invisible injuries. He said one fellow medical officer -- whom he did not identify -- told him that he feared creating "another John Kerry" by giving out the Purple Heart for concussions.
During the 2004 presidential campaign, some political opponents mocked Sen. Kerry, D-Mass., the Democratic nominee, for receiving three Purple Hearts for shrapnel wounds he got during the Vietnam War, which critics deemed too minor to deserve recognition. In the last of these actions, Kerry also received a Bronze Star.
"We need to give these troops" the Purple Hearts "they rightly deserve," Neely wrote.
Neely declined to comment for our story. But a fellow officer said that "no more John Kerrys" became a catchphrase among some medical officers in Iraq who felt that mild traumatic brain injuries were not serious enough to merit Purple Hearts.
The officer, who did not want to be named for fear of damaging his career, said commanders often relied on technicalities to block awards. For instance, the military defines a "medical officer" as a physician with officer rank. That means that soldiers treated by nurses or combat medics would not necessarily qualify.
"They were trying to find ways not to give the Purple Heart," the official said. "There was a lot of semantics going on."
Russell, the Army neuropsychologist, and Col. Rodney Coldren, an Army epidemiologist, alluded to this attitude at the 2009 National Academy of Neuropsychology conference. They told the audience that the Purple Heart "clouds everything" in diagnosing concussions in the field.
Coldren, who traveled to Iraq in 2009 to study testing for mild traumatic brain injuries, said he found "vast under-diagnosis" of concussions, and not just because electronic reporting systems were failing.
"Another issue we found in Iraq as far as under-diagnosis is the issue of the Purple Heart," Coldren said, according to a transcript of his remarks obtained by NPR and ProPublica. "There was a push by higher level commanders to not be seen to be giving these out for just any old injury."
When contacted by NPR and ProPublica, both Coldren and Russell declined through spokesmen to comment on their remarks.
Veterans groups that focus on the Purple Heart support awarding it in cases of concussions, as the regulations spell out.
"A guy rolls over an IED and maybe the concussion isn't so bad, but he can't go back to work the next day," said John E. Bircher III, spokesman for the Military Order of the Purple Heart, a congressionally chartered veterans group. "He's entitled to a Purple Heart, (just like) the guy who gets hit by shrapnel and gets six stitches and goes back to work right away."
Other veterans groups expressed anger that soldiers with brain injuries were not being recognized for their wounds.
"It's an outrage," said Paul Sullivan, a former Department of Veterans Affairs official who now heads Veterans for Common Sense, an advocacy group. "What I'm afraid of is that the military intentionally is concealing casualties in order to conceal the enormous human costs of the Iraq and Afghanistan war."
Struggle for recognition
The system for awarding Purple Hearts can be opaque, especially for soldiers in war zones. They often do not get a response in writing, receiving only verbal notifications that they have been turned down. Even when they do get letters, the reason for denial can be vague, such as a lack of proper documentation.
NPR and ProPublica contacted more than a dozen officers to determine who, exactly, had turned down the Purple Heart applications of Scheller, Hopkins, Junge and other soldiers. The officers either did not comment, or said they could not recall the cases.
Soldiers turned down for the Purple Heart can appeal, but face a grinding administrative battle to reverse the decision.
If they have no documentation of their wounds, they must find witnesses and gather sworn statements, an especially daunting task for those who have cognitive deficits as a result of brain injuries.
After surviving two roadside blasts in Iraq in 2008, Capt. Jonathan Brooks fought for 14 months to receive a diagnosis confirming that he had suffered a concussion that resulted in lingering symptoms.
His wife, Jayna Moceri Brooks, decided to apply for a Purple Heart. The process was so complex that she co-founded a group, Recognize the Sacrifice, to help other soldiers apply for the medal.
In some cases, soldiers she is helping have spent more than two years working through the appeals process. (The Army Review Boards Agency still gets applications to honor soldiers injured in World War I and World War II.)
Brooks, a registered nurse who has worked in military hospitals, said the recognition was worth the effort.
"A Purple Heart medal would symbolize support from the Army and from the greater civilian community as we endure the frustrations and hardships of living with a (traumatic brain injury). It's pretty lonely without having that official recognition and support," Brooks said. "It's exhausting to have to fight and ask for everything ourselves."
Last year, Rep. Bill Pascrell, D-N.J., the co-chairman of the Congressional Brain Injury Task Force, demanded that the military explain how it decides whether soldiers with mild traumatic brain injuries are awarded the Purple Heart.
The military's report, delivered in June, noted that the Army and other service branches had different requirements. The Marine Corps, for instance, requires that a service member must have been knocked unconscious to receive the Purple Heart for mild traumatic brain injury.
Yet, according to an internationally accepted medical definition, a person can suffer a mild traumatic brain injury with or without a loss of consciousness.
Pascrell said he is pressing for consistent regulations regarding the Purple Heart. He called the military's report "unacceptable."
"There are people being overlooked because of the criteria being so vague," Pascrell said. "We have let too many of our soldiers fall through the cracks and it's not acceptable."
Michelle Dyarman is one of those soldiers. A major in the Army reserves, Dyarman was injured by two roadside bombs in Iraq in 2005. After years of fighting with the military, she was eventually diagnosed as having suffered a mild traumatic brain injury that caused lasting cognitive problems. Dyarman still has trouble concentrating, following directions and remembering words.
She is still fighting. Commanders have repeatedly denied her application for a Purple Heart, sending her into a bureaucratic maze. The Purple Heart, she said, would prove to everyone what she already knows: She sacrificed for her country.
"I know I'm not the only one it happened to," she said. "It's very frustrating. It's very disappointing."
Pentagon Spokesman Wrong on Purple Heart
On Thursday, we published a story that said the Army isn't awarding Purple Hearts to some soldiers who suffered mild traumatic brain injuries in Iraq.
We found e-mails showing that some top medical commanders don't think the injury is serious enough to merit the honor, even though Army regulations [PDF] make it clear that soldiers with such head trauma are eligible for the award. Top brass acknowledged that commanders had mistakenly denied the honor to soldiers in the past, but said things were getting better. "We are moving in the right direction to fix this," Gen. Peter Chiarelli, the Army's second-in-command told us.
They've still got a ways to go, if a slip-up by the Pentagon's top spokesman is anything to go by.
After our story ran, Geoff Morrell, spokesman for Defense Secretary Robert Gates, was asked a question about the Purple Heart at the daily Pentagon press briefing. He told an ABC News reporter that the Purple Heart "has not been" authorized for mild traumatic brain injuries. Also known as concussions, such head wounds typically leave no visible signs of damage, though they can result in long-term cognitive impairment.
"I don't think that people think this is an appropriate medal for those types of injuries," he said.
That's not what Army regulations say, however. As far back as the 1950s, the regulations have contained an official list of wounds that "clearly justify" the Purple Heart, the nation's oldest military honor. One of them: "Concussion injuries caused as a result of enemy generated explosions."
The Pentagon has corrected Morrell's mistake. The official transcript contained this addition: "Correction: Each service ensures members who sustain a concussion/mild TBI are awarded the Purple Heart if the two basic Purple Heart criteria are met: wound was the result of enemy action or occurred in action with the enemy, and the wound required treatment by a medical officer."
So that settles it. Now we'll see how the Army responds to the soldiers we interviewed, who have battled unsuccessfully to receive the Purple Heart despite well-documented wounds. Morrell didn't immediately respond to requests for comment.
Congresswoman Calls for Review of Purple Heart Decisions
In response to reports by NPR and ProPublica, a congresswoman on the House Armed Services Committee is urging the Pentagon to review decisions to deny Purple Hearts to some soldiers suffering from mild traumatic brain injuries.
In a letter sent Wednesday to Secretary of Defense Robert Gates, Rep. Chellie Pingree, D-Maine, called it "unacceptable" that Army commanders have turned down soldiers who met criteria for award of the Purple Heart, which recognizes soldiers wounded or killed in combat.
"It's absolutely heartbreaking to hear the stories of these injured veterans, whose families say they just aren't the same person since surviving a blast," Pingree said in a statement. "Just like those who suffer bullet wounds, their injuries rightfully deserve the recognition the Purple Heart symbolizes. Denying them the honor they are due because their injuries are on the inside instead of the outside is unacceptable and downright demeaning."
Army regulations [PDF] make clear that mild traumatic brain injury, also known as concussion, is among the wounds that entitle soldiers to the Purple Heart. Those suffering concussions must have received the wound during hostile action and received treatment from a medical officer.
Our story found instances in which soldiers were turned down despite well-documented blast wounds and medical treatment. We uncovered e-mails that showed some top Army medical commanders doubted whether mild traumatic brain injuries were serious enough to merit the Purple Heart. Such injuries are difficult to detect and often leave no visible signs of damage to the brain. Most soldiers recover quickly, but a minority endure lingering problems with memory, focus and concentration.
In a sign of confusion over the issue, the Pentagon's chief spokesman, Geoff Morrell, said at a press briefing last week that soldiers with concussions were not eligible for the Purple Heart. The transcript of his remarks was later corrected.
"While not every service member exposed to IED blasts will suffer the lasting consequences associated with TBI, every service member who is exposed to an enemy generated explosion and receives medical attention should receive the Purple Heart," Pingree wrote.
An Army spokesman did not immediately return a request for comment. Gen. Peter Chiarelli, the Army's vice chief of staff, acknowledged in interviews that some commanders and medical officials did not award the Purple Heart for concussions.
He asked for a legal review after NPR and ProPublica showed him a 2008 policy [PDF] issued by the top medical commander in Iraq, which appeared to contradict Army regulations by restricting which soldiers could receive the award. That review was still ongoing as of last week.
Update: A spokesman for the Army said Chiarelli said he had not seen Pingree's letter.
How Our FOIA Request Was Blocked, and Why We’re Still Pursuing It
In May 2009, the Pentagon asked a nonprofit company to study cognitive rehabilitation therapy, a painstaking and often expensive treatment program to help soldiers with brain injuries relearn tasks of daily living.
The $21,000 study, conducted by Pennsylvania-based ECRI Institute, found limited evidence that the therapy is effective. That tiny contract had a profound impact on tens of thousands of people who have suffered brain damage while serving in Afghanistan and Iraq. Tricare, the health plan for troops and many veterans, relied on its findings to deny coverage for the therapy.
Leading experts on brain injuries sharply criticized Tricare's decision, arguing that cognitive rehabilitation was a well-proven technique whose efficacy had been established by numerous scientific studies. They noted that expert committees convened by the Pentagon and the National Institutes of Health had unanimously agreed on the value of cognitive rehabilitation as a treatment.
To examine the basis of Tricare's decision, ProPublica and NPR filed a Freedom of Information Act request in March 2010 requesting a copy of the ECRI study and "all external and internal" reviews of its validity. We also asked for a copy of the contract between Tricare and the institute.
In response, officials at ECRI and Tricare have given us contradictory denials and explanations. For instance, seven months later, Tricare provided a copy of the study but said in a written letter that "no written internal review ... exists." Tricare acknowledged the existence of "external reviews" but said they would not provide them since "they were submitted voluntarily, were not contracted by" the Department of Defense "and the content is not owned by" the Department of Defense.
At the same time, a Tricare FOIA officer told ProPublica and NPR that a copy of the contract had been sent to ECRI for review. Private firms are allowed to review government contracts prior to public release to make sure that they do not contain confidential business information.
We are appealing that denial. Here's why.
ProPublica and NPR have learned that five brain rehabilitation experts conducted reviews of the Tricare study. Those reviews, according to people who have seen them, criticized the ECRI study.
Two of those reviews were called for in ECRI's contract with the Pentagon. According to ECRI officials, both were critical of the study's findings and methodology. ECRI said it stood by its report, and called the criticism part of normal scientific debate.
ECRI officials said they were willing to provide copies of those reviews to ProPublica and NPR, but that Tricare told the company that it could not do so because the reviews were owned by Tricare -- a direct contradiction of Tricare's statement to us.
"ECRI Institute declined requests to provide copies of the external reviews because, as required deliverables under ECRI Institute's contract with Tricare, they are the property of Tricare," wrote Vivian Coates, an ECRI vice president.
In addition, ECRI spokesman Laurie Menyo said that ECRI had never been asked to review a copy of the contract -- contradicting the Pentagon's statement that its release was being delayed while the company examined it.
"Our legal counsel has no record of being contacted by FOIA regarding any documentation," Menyo said in an e-mailed statement.
ProPublica and NPR has learned that Tricare asked for three additional peer reviews after it received the ECRI study. In an interview, Capt. Robert DeMartino, who directs Tricare's behavioral health department, acknowledged that these reviews were "of concern." He said Tricare planned to conduct further studies of cognitive rehabilitation.
Although Tricare did not release these reviews, ProPublica and NPR obtained copies of them. All three attacked the Tricare study in strong terms, calling it "deeply flawed," "unacceptable" and "dismaying."
One top scientist termed the ECRI study a "misuse" of science designed to deny treatment for service members. "Reviewing this report brings to mind the stance taken by the tobacco companies many years ago with regard to the relationship between cigarette smoking and various types of cancer," wrote Wayne Gordon, director of rehabilitation psychology and neuropsychology servicesat Mt. Sinai School of Medicine in New York. "They chose to turn their back on the existing evidence."
A Pentagon spokeswoman declined comment on Tricare's decision not to release the reviews, or their apparent failure to send a copy of the contract for review, citing the pending appeal.
"It is inappropriate for us to make any comments concerning the appeal or the processing of the initial FOIA request by Tricare," wrote Cynthia Smith, a Pentagon spokeswoman.
ProPublica and NPR will post the results of the decision when they are available.
Pentagon Health Plan Won’t Cover Brain-Damage Therapy for Troops
A version of this story was aired on NPR's "All Things Considered." Listen to the audio of that broadcast below:
During the past few decades, scientists have become increasingly persuaded that people who suffer brain injuries benefit from what is called cognitive rehabilitation therapy -- a lengthy, painstaking process in which patients relearn basic life tasks such as counting, cooking or remembering directions to get home.
Many neurologists, several major insurance companies and even some medical facilities run by the Pentagon agree that the therapy can help people whose functioning has been diminished by blows to the head.
But despite pressure from Congress and the recommendations of military and civilian experts, the Pentagon's health plan for troops and many veterans refuses to cover the treatment -- a decision that could affect the tens of thousands of service members who have suffered brain damage while fighting in Iraq and Afghanistan.
Tricare, an insurance-style program covering nearly 4 million active-duty military and retirees, says the scientific evidence does not justify providing comprehensive cognitive rehabilitation. Tricare officials say an assessment of the available research that they commissioned last year shows that the therapy is not well proven.
But an investigation by NPR and ProPublica found that internal and external reviewers of the Tricare-funded assessment criticized it as fundamentally misguided. Confidential documents obtained by NPR and ProPublica show that reviewers called the Tricare study "deeply flawed," "unacceptable" and "dismaying." One top scientist called the assessment a "misuse" of science designed to deny treatment for service members.
Tricare's stance is also at odds with some medical groups, years of research and even other branches of the Pentagon. Last year, a panel of 50 civilian and military brain specialists convened by the Pentagon unanimously concluded that cognitive therapy was an effective treatment that would help many brain-damaged troops. More than a decade ago, a similar panel convened by the National Institutes of Health reached a similar consensus. Several peer-reviewed studies in the past few years have also endorsed cognitive therapy as a treatment for brain injury.
Tricare officials said their decisions are based on regulations requiring scientific proof of the efficacy and quality of treatment. But our investigation found that Tricare officials have worried in private meetings about the high cost of cognitive rehabilitation, which can cost $15,000 to $50,000 per soldier.
With so many troops and veterans suffering long-term symptoms from head injuries, treatment costs could quickly soar into the hundreds of millions, or even billions of dollars -- a crippling burden to the military's already overtaxed medical system.
The battle over science and money has made it difficult for wounded troops to get a treatment recommended by many doctors for one of the wars' signature injuries, according to the NPR and ProPublica investigation. The six-month investigation was based on scores of interviews with military and civilian doctors and researchers, troops and their families, visits to treatment centers across the country, confidential scientific reviews and documents obtained under the Freedom of Information Act.
"I'm horrified," said James Malec, research director at the Rehabilitation Hospital of Indiana and one of the reviewers of the Tricare study. "I think it's appalling that we're not knocking ourselves out to do the very best" for troops and veterans.
Defense Secretary Robert Gates, who has complained over the past year about the growing cost of the Pentagon's health care budget, declined a request for an interview. George Peach Taylor, the newly appointed acting assistant secretary of defense for health affairs, the top ranking Pentagon health official, also declined repeated interview requests. Tricare officials defended the agency's decision not to cover cognitive rehabilitative therapy and said it was not linked to budget concerns.
Capt. Robert DeMartino, a U.S. Public Health Service official who directs Tricare's behavioral health department, said Tricare is mandated to ensure the quality, consistency and safety of medical care delivered to service members.
He said those standards can be difficult to meet with cognitive rehabilitation. Therapists design highly individualized treatment plans, often relying on a variety of different techniques. The holistic approach and lack of standardization makes it hard to measure the effects of the therapy, he added.
DeMartino noted that the agency covers some types of treatment considered part of cognitive rehabilitative therapy. For instance, Tricare will pay for speech and occupational therapy, which can play a role in cognitive rehabilitation.
DeMartino said cost played no role in the agency's decision, calling such a suggestion "completely wrong." He defended the agency's studies of cognitive rehabilitation, calling them objective scientific reviews designed to ensure troops and retirees receive the best treatment possible.
Cognitive rehabilitation therapy "is a new field for us," DeMartino said. "We don't know what it is. That's really an important thing. You don't want to send people out when you don't know what treatment they're going to get and what the services are going to be."
Officials at the Pentagon are themselves divided on the value of the treatment. A handful of military and veteran facilities provide cognitive rehabilitation therapy, though most do not have the capacity or offer programs of limited scope.
Tricare was designed to fill in such gaps in the military health system by allowing troops and veterans access to civilian medical providers. But since Tricare has a policy against covering cognitive rehabilitation, service members and retirees who seek treatment at one of the nation's hundred of civilian rehabilitation centers could have their claims denied, or only partly paid.
The contradictory policies have resulted in unequal care. Some troops and their families have relied upon high level contacts or fought lengthy bureaucratic battles to gain access to civilian cognitive rehabilitation programs which provide up to 30 hours of therapy a week. Soldiers without strong advocates have been turned away from such programs, or never sought care, due to Tricare's policy of refusing to cover cognitive rehabilitation therapy.
As a result, many soldiers, Marines and sailors with brain injuries wind up in understaffed and underfunded military programs providing only a few hours of therapy a week focused on restoring cognitive deficits.
Sarah Wade's husband, Ted, was a sergeant with the 82nd Airborne Division when a roadside bomb tore through his Humvee in February 2004. The blast severed his right arm above the elbow, shattered his body and left him with severe brain damage.
After the military medically retired her husband later that year, Wade struggled to find appropriate care for him. The closest VA hospital set up to handle such complex injuries was in Richmond, Va., a 320-mile drive from their home in North Carolina.
Tricare, however, would not pay for cognitive rehabilitation at a nearby civilian program. Wade, who once worked as an intern on Capitol Hill, turned herself into a one-woman lobbyist on her husband's behalf. She called her representatives and met with senior VA and DOD officials. She testified before Congress, met President George W. Bush and Gates, and was recently invited to the White House by President Barack Obama for a bill signing ceremony.
Wade managed to set up a special contract between the VA and a local rehabilitation doctor to help her husband. But now she wants to move back to Washington, D.C., to be closer to family.
She must begin her fight all over again -- more phone calls to Tricare, more visits to government offices, more battles to get Ted Wade the care he needs.
"We go to Capitol Hill like some people go to the grocery store," Wade joked one afternoon during a recent visit to Washington. "If we can't figure it out, then probably nobody can."
Brain Campaign
The campaign to persuade Tricare to cover cognitive rehabilitation therapy began in earnest after the scandal at Walter Reed Army Medical Center in Washington in 2007. News reports featured brain-damaged soldiers living in squalid conditions and receiving substandard care.
The Brain Injury Association of America, a grassroots advocacy group for head trauma victims, started lobbying Congress and the Defense Department to order Tricare to cover rehabilitation for service members.
The campaign was a natural extension of the association's mission. Each year, more than 1.4 million American civilians suffer brain injuries in car accidents, strokes and other medical emergencies. They and their families often have to battle private insurance companies for cognitive rehabilitation.
The insurance industry is divided: Five of 12 major carriers will pay for cognitive rehabilitation therapy for head trauma, according to Tricare's study. Aetna, United Healthcare and Humana cite national evidence-based studies and industry-recognized clinical recommendations that point to the therapy's benefits.
The federal Centers for Medicare and Medicaid Services does not have a single national policy on cognitive rehabilitation. Instead, it leaves decisions to local contractors, often insurance carriers who process claims for the agency. The contractors are able to provide the therapy case by case, so long as they determine the treatment is "reasonable and necessary," a Medicare spokesman said.
"The totality of the evidence appears to support the value of cognitive rehabilitation for people with traumatic brain injury in improving their function," said Robert McDonough, the head of clinical policy at Aetna. "We feel on balance the evidence leads us to conclude that cognitive rehabilitation is effective."
Carriers and doctors providing the service can point to a long list of medical associations and scientific studies backing the effectiveness of cognitive therapy: The National Institutes of Health; the National Academy of Neuropsychology and the British Society of Rehabilitation Medicine, among others, have weighed in supporting the treatment.
Armed with such evidence, brain injury association lobbyists did not have much trouble finding support in Congress. By 2008, more than 70 House and Senate members had signed letters to Gates asking him to support funding for cognitive rehabilitation therapy. Then-Sen. Obama led a group of 10 senators urging Tricare to pay for therapy.
They noted that the Pentagon and the VA have improved their efforts to treat brain injury, including increases in the number of doctors and therapists available at facilities.
But the military needed to do more, they said. They wrote that Tricare should cover cognitive rehabilitation so all troops "can benefit from the best brain injury care this country has to offer."
"Given the prevalence of TBI among returning service personnel, it is difficult to comprehend why the military's managed healthcare plan does not cover the very therapies that give our soldiers the best opportunities to recover and live full and productive lives," the letter said.
A response letter from the Pentagon told the representatives that Tricare officials had not been convinced by available evidence. "The rigor of the research ... has not yet met the required standard," wrote Gordon England, then the deputy defense secretary.
Everyone Agrees
On an unusually hot spring day in April 2009, 50 of America's leading brain specialists gathered for two days in a sterile hotel ballroom in suburban Washington, D.C.
The Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury, the Pentagon's lead program for the treatment of brain injury, convened the conference to help settle the debate about cognitive rehabilitation therapy.
The participants were top researchers and doctors from the military and civilian world: neurologists, neuropsychologists, psychiatrists, therapists, family doctors and rehabilitation experts.
After two days of discussion, the group hammered out a consensus report, representing the combined wisdom of the field. Their unanimous conclusion: Cognitive therapy improved the thinking skills and quality of life for people suffering from severe and moderate head injuries. Troops with lingering problems from a mild traumatic brain injury, or concussion, also could benefit from the therapy, the experts said.
The consensus was not binding. But those in attendance believed that their opinion -- based on the decades of combined clinical experience and academic study present in the room -- would lead to troops' receiving better treatment.
"When you get the right people in the right room at the right time, you'd expect it would influence the decision makers," said Maria Mouratidis, chairwoman of psychology and sociology at the College of Notre Dame in Baltimore and a conference participant.
Shortly after the conference ended, however, a handful of top officials from the military's medical system met to discuss the findings at Tricare's headquarters, an anonymous sprawl of office buildings in Falls Church, Va., known as Skyline 5.
One person familiar with the discussion, who did not want to be identified for fear of reprisal, said money was part of the debate.
Official Pentagon figures show that 188,000 service members have suffered brain injuries since 2000. Of those, 44,000 suffered moderate or severe head injuries. Another 144,000 had mild traumatic brain injuries. However, previous ProPublica and NPR reports showed that number likely understates the true toll by tens of thousands of troops. Some estimates put the number of brain injuries at 400,000 service members.
Mild traumatic brain injuries are the most common head trauma in Iraq and Afghanistan. Commonly caused by blast waves from roadside bombs, such injuries are defined as a blow to the head resulting in an alteration or loss of consciousness of less than 30 minutes. Studies suggest that while most troops with concussions heal quickly, some 5 percent to 15 percent go on to suffer lasting difficulties in memory, concentration and multitasking.
For the military's health system, the costs of treating brain damaged soldiers with cognitive rehabilitative therapy added up quickly. If tens of thousands of service members and veterans were authorized to receive such treatment, the bill might be in the billions, using high-end estimates for the cost of treatment from the Brain Injury Association.
The costs could swell the Pentagon's annual $50 billion health budget -- at a time when Gates has said the military is being "eaten alive" by skyrocketing medical bills.
Tricare "is basically an insurance company. They'll take no action to provide more service," said the person familiar with the conversation, who would only discuss it in general terms. "If they do it, it's an enormous cost."
At the meeting following the consensus conference, the person said, Tricare staked out its own position: "They had already decided not to do it," the person said.
NPR and ProPublica contacted two others who attended the meeting. Jack Smith, Tricare's acting chief medical officer, said through a spokesman that he could not recall the meeting, but "can't say for sure there wasn't one." Rear Adm. David J. Smith, the joint staff surgeon, declined comment through a spokesman.
The Contract
Soon after the meeting, Tricare sprang into action. In May 2009, records show, it issued a $21,000 contract to the ECRI Institute, a respected nonprofit research center best known for evaluating the safety of medical devices.
The contract called for ECRI to review the available scientific literature to weigh the evidence for whether cognitive rehabilitation therapy helped improve patients with traumatic brain injuries.
Tricare routinely hires contractors to carry out assessments to help determine which medical treatments to fund. But in selecting ECRI, Tricare had a pretty good idea of the response it would receive. ECRI had conducted a similar review for Tricare in 2007 that cast doubts on the evidence supporting cognitive rehabilitation therapy.
To carry out the new review, ECRI followed its standard protocol. It chose to include only randomized, controlled studies. Such studies randomly divide patients into groups that receive different treatments in order to compare their effects.
ECRI gave more credence to blind studies, meaning that patients did not know whether they were receiving genuine therapy or a placebo -- a fake treatment. Blinding reduces bias and is considered one of the most rigorous standards that can be used in scientific testing.
ECRI also excluded studies deemed irrelevant; those studies with fewer than 10 patients; and studies where 15 percent or more of the patients were injured from a nontraumatic blow, such as stroke.
The criteria resulted in the elimination of much of the published scientific literature on cognitive rehabilitative therapy. Before applying the protocol, ECRI identified 318 articles as potential sources of information about cognitive rehabilitative therapy. The firm's final report examined 18.
Based on this limited pool, ECRI graded the evidence for the benefits of cognitive therapy as being "inconclusive" or offering only "low" or "moderate" support of improvement in patients' cognitive functions.
The final report, delivered to Tricare in October 2009, noted some areas of benefit. For instance, "tentative" evidence showed cognitive therapy significantly improved quality of life for brain-damaged patients.
ECRI's review wasn't limited only to science. The review noted one study that found that comprehensive cognitive rehabilitative therapy could cost as much as $51,480 per patient. By contrast, sending patients home from the hospital to get a weekly phone call from a therapist amounted to only $504 per patient.
Overall, the report concluded, the evidence for most benefits from cognitive rehabilitation therapy remained inconclusive, especially when compared to cheaper programs.
"The evidence is insufficient to determine if comprehensive, holistic (cognitive rehabilitation therapy) is more effective than less intensive care" in helping patients, the 2009 report concluded.
Tricare Criticized
By the summer 2009, ECRI researchers had finished a draft of the study. ECRI, later joined by Tricare, asked outside scientific experts to review it.
The reviews, according to interviews and copies obtained by NPR and ProPublica, were uniformly critical.
(NPR and ProPublica obtained a copy of the ECRI reports through the Freedom of Information Act. However, Tricare denied access to reviews of the reports. ProPublica and NPR have appealed the request, but obtained copies of the reports and information on the reports from sources.)
The reviewers acknowledged that more research was needed on cognitive rehabilitation therapy. However, they noted that the Tricare report ran counter to several other so-called meta-analyses, which combine multiple, individual scientific studies to achieve greater statistical reliability.
For instance, a 2005 article in the Archives of Physical Medicine and Rehabilitation, a peer-reviewed journal that is one of the mostly widely respected in the field, examined 258 studies. It concluded that "substantial evidence" supported cognitive rehabilitation. The review included 46 randomized control studies -- more than double the number in the Tricare study.
Reviewer Keith Cicerone, a leading civilian researcher who runs the JFK Johnson Rehabilitation Institute's Center for Head Injuries in New Jersey, disputed Tricare's contention that the treatment was new and untested.
"We have a significant body of evidence describing cognitive rehabilitation and showing what works in cognitive rehabilitation," Cicerone said. "The idea that cognitive rehabilitation is new and untested is simply not true. It's got a better evidence base than most things that we do in rehabilitation."
Asked to explain in plain terms, Cicerone grew animated: "The arguments that are being made against" cognitive rehabilitation "in terms of the level of research that has been conducted are hooey," he said. "It is baloney."
The outside experts also attacked Tricare and ECRI for relying upon a methodology that ruled out important research. ECRI's protocols, they acknowledged, are well-suited for drug studies, where it is easy to prevent patients from knowing which pill they are receiving.
But ECRI's protocols do a poor job in assessing rehabilitation therapy where patients and doctors constantly interact in face-to-face treatment sessions. Other well-accepted methodologies, they said, have been designed to examine the benefits of therapeutic interventions.
They also questioned the reasons for excluding studies with a small number of patients, or with differing causes for brain injury, since a stroke can produce the same types of symptoms as a blow to the head.
Malec, the research director at the Rehabilitation Hospital of Indiana, said Tricare's study sounded like it came from a private insurance company seeking to cut costs. His review said that Tricare's study "fails to represent the evidence relevant to evaluating the effectiveness of cognitive rehabilitation after traumatic brain injury."
In an interview, he said Tricare's demand for conclusive evidence was understandable, but ill-advised. While research continues, existing evidence indicates that the therapy helps, with no studies showing that it harms troops.
"They missed the forest for the trees. They missed the big picture," he said.
Some of the researchers accused Tricare of using ECRI's strict assessment protocols as a cover to justify denying troops' coverage.
Wayne Gordon, director of rehabilitation psychology and neuropsychology services at Mt. Sinai School of Medicine in New York, called the review "dismaying" and "unacceptable." He compared it to tobacco companies that dismissed studies that showed a link between smoking and cancer.
"The ECRI Institute seems to be stating that, while sufficient evidence exists for there to be consensus among diverse groups that cognitive rehabilitation is a useful service, this evidence is 'not good enough' for Tricare," wrote Gordon, who declined to explain his comments further in an interview. He wrote that the ECRI study was "designed to reach a negative conclusion."
ECRI also asked two additional researchers to examine the report, John Corrigan, director of the Ohio Valley Center for Brain Injury Prevention and Rehabilitation in Columbus, and John Whyte, the director of Moss Rehabilitation Research Institute in Pennsylvania, both leading researchers in the field.
Both men declined to comment, citing their contractual obligations with ECRI, and Tricare declined to release their reviews. People familiar with their contents said Corrigan and Whyte closely mirrored the views of their fellow critics. They recommended that ECRI use a different method to judge studies of cognitive therapy, but the institute refused.
ECRI "said thank you very much, but we're not changing anything," said one person familiar with the review process.
More Studies, More Waiting
In an interview, ECRI Institute officials defended their firm's methodology. The system is designed to provide a rigorous review free from researchers' bias, they said.
Karen Schoelles, ECRI's medical director for the health technology assessment group, acknowledged that some of the institute's criteria -- such as accepting only studies with 10 or more patients -- were "arbitrary." But she said they were widely accepted in the assessment industry.
She also noted that Tricare officials were aware of the criteria and made no attempt to change or adjust them. Tricare used ECRI Institute for almost 10 years to carry out health reviews, though the agency recently terminated the contract and selected a new firm to carry out assessments.
Cognitive rehabilitation "may be on to something," Schoelles said. "But it needs more research."
Schoelles acknowledged that ECRI's own reviewers had criticized the report. ECRI offered to provide copies of the reviews, but later said that Tricare ordered them not to release them.
Stacey Uhl, the lead researcher on the review, said the criticism did not change her view that randomized controlled trials were the best way to assess the quality of evidence.
She noted the review found evidence that cognitive therapy did help in some way and said she would not rule out seeking such care for a loved one.
"I as a parent would want my child to receive all available therapies," she said.
DeMartino, the Tricare official who commissioned the report, acknowledged the outside reviewers had "very, very strong opinions" that were "of concern."
He said Tricare was conducting a review to determine whether ECRI's techniques were best suited to measure cognitive therapy's benefits. He denied submitting cognitive therapy to overly-strict review standards.
"You get what you ask for," DeMartino said. "They tell us what they're going to give us, and it's our job to sort of say, 'Okay, we understand that within the limitations of their methodology, this is the information that we get.'"
He added: "The better the information you have, the better that you can move forward and do the best thing." The Tricare reports, coupled with high cost projections, ended the legislative push to get cognitive rehabilitation for service members and veterans.
Last year, Congress ordered the Pentagon to conduct further studies to review the effectiveness of the therapy, but those studies have not yet begun and results are not expected for several years.
Tricare said it would conduct regular reviews to monitor developments in the field. DeMartino first said Tricare would carry out a new review beginning in September. A spokesman later clarified that the National Academy of Sciences Institutes of Medicine would perform the review. It is scheduled to be completed by the end of 2011.
Susan Connors, president of the brain injury association, said she was stunned by the need for legislation at all. As the Pentagon conducts yet more studies, thousands of troops and veterans may be going without the best known treatment available. Thousands more would have to rely on military hospitals or veterans clinics far from their homes, or with substandard programs. The Tricare refusal shut down access to the hundreds of civilian rehabilitation clinics nationwide.
"I'm very disappointed by the resistance," she said. "The military should want to do this."
Struggling for Care
Tricare's stance has not made it impossible to get cognitive rehabilitative. But it has discouraged civilian clinics from treating soldiers.
In interviews, several clinic owners and medical directors described their frustrations.
On some occasions, they were paid after developing relationships with individual Tricare claims processors or case managers, only to have the arrangements fall apart if the person left.
"We have tried to get Tricare and just beat our head against the wall," said Brent Masel, the president of the Transitional Learning Center in Galveston, Texas. "It took forever to get paid. It was always a fight."
Mark Ashley, the president of the Centre for Neuro Skills, a chain of rehabilitation clinics, said Tricare and other insurance providers were unwilling to pay because those with brain injuries can often perform basic functions that let them get through their daily lives.
They are "able to walk around, able to maneuver, but can't function cognitively in a manner that's safe, appropriate or competent," said Ashley, a past president of the brain injury association. "We can fix much of that, but it takes an exhaustive amount of time and effort. That's where the payers are out of touch."
One of the nation's top brain injury centers set up a charity program to help cover gaps left by Tricare. Susan Johnson, who runs Project Share at the Shepherd Center in Atlanta, said Tricare pays only about 40 cents of each dollar of care provided for the type of comprehensive program that the clinic has found successful. The rest comes from Bernie Marcus, a billionaire philanthropist, and income from inpatient services.
"These guys go and they put their lives on the line and we put them in this situation that's difficult for some and less difficult for others to get care," Johnson said. "I find it frustrating."
Other clinic owners said they were able to game the system by providing cognitive therapy, but billing for other Tricare-covered services -- putting them at risk of being accused of false billing.
One clinic manager acknowledged being "creative" when submitting bills to Tricare. He said that he submitted bills to Tricare for occupational therapy when the treatment focused more on improving memory.
"They won't pay for this, but they will pay for that," said the manager, who did not want to be identified for fear of damaging his ability to receive payments. "You just have to figure out how to work the system."
Soldiers and families agreed that Tricare's stance has made getting care a battle.
Sarah Wade said she patched together adequate care for Ted, arranging for him to go to a VA hospital for some services and to travel to Walter Reed Army Medical Hospital for others.
Tricare would have paid for some things, such as a physical therapist to help him learn to walk again. But she has had no luck trying to persuade Tricare to pay to treat his brain injury.
In frustration, Wade personally visited a high-ranking official at the Veterans Affairs Department. He, in turn, ordered a VA hospital to fund a special contract with a local civilian rehabilitation doctor near the Wades' North Carolina home.
"Yes, we have been able to get [cognitive rehabilitation] paid for, but it's been with a lot fighting, red tape, and bureaucracy," Sarah Wade said. "It's his greatest injury and the one that impacts his life the most, that impacts his ability to be a human." She added, "It shouldn't be this hard."
The Wades credit the rehabilitation that Ted has received with markedly improving his cognitive problems. After his 2004 injury, Ted spent months regaining consciousness. Doctors were unsure about his mental state, not certain he would ever talk or even think rationally.
Today, Ted speaks in slow, sure sentences, even cracking jokes. He can make decisions -- choices that seem simple enough to someone with normal cognitive skills, but which often stymie those with brain injury.
He knows, for example, to buy cherry tomatoes at the store rather than big tomatoes, which are hard for him to chop and slice with only one arm. He can read through a menu, and pick food that's nutritious. He can wash and fold his own laundry.
One recent day after dining at a Mexican restaurant in Washington, Ted smiled when Sarah reminded him that he was once unable to figure out whether he liked hot sauce on his tacos.
"It's been a long, slow process," he said.
For Brain-Injured Soldiers, Top Quality Care From a Philanthropist, not the Pentagon
A version of this story was aired on NPR's "Morning Edition". Listen to the audio of that broadcast below:
One afternoon this fall, Bobby McKinney hunched over a coffee table with a clear glass surface. A lamp with a bare light bulb illuminated it from below. Pencil in hand, the former Marine traced the pattern for a tattoo across delicate paper, a swirling, intricate design reminiscent of a Celtic cross.
McKinney's small apartment faded from his thoughts: The closet filled with shirts and pairs of jeans, hung three inches apart, all facing exactly the same direction, the way the Marines had taught him. The box packed with a dozen brown plastic medicine bottles. The worn couch that he slept on instead of the bed. The eraser board on his refrigerator where he had scrawled "A coward dies a 1,000 deaths. A warrior dies one."
Suddenly, a nurse's aide knocked on the door. Had he checked the oven? McKinney leapt up and ran to the kitchen, pulling out a tin of brownies on the point of burning.
"I guess I was just very focused on the tattoo design," he told a counselor later, pushing a camouflage baseball cap back on his head. "I set the alarm. I guess I just didn't hear it."
"Try to work on one thing at a time," she told him. "Multitasking is just asking the brain to do two or three things not too well."
McKinney, 29, nodded in agreement. It seemed so obvious once she said it. But his mind -- the mind that once helped sniper teams in Iraq, that navigated battlefield maps and complex rules of enemy engagement -- had just not come up with the idea to do one task instead of many. "When you think about it, it kinda makes sense. But I wouldn't think about it on my own," he said.
McKinney is an Iraq war veteran who suffered multiple concussions, also known as mild traumatic brain injuries. Bomb blasts jarred his brain, leaving him with no outside scars, but with nagging mental problems. His short-term memory is bad. He moves slowly through ordinary chores. He gets disoriented easily, and can't find his way to the home that he has lived in for months without the aid of a GPS.
A farm boy fond of the Georgia Bulldogs and chewing tobacco, McKinney has pinned his hopes for recovery on cognitive rehabilitation therapy, a subtle and complex treatment for a subtle and complex injury. Doctors and studies have shown that the therapy helps soldiers. But the Pentagon's primary health plan for soldiers and seriously wounded veterans, called Tricare, will not cover the treatment, saying it is still unproven.
To see what cognitive therapy looked like, ProPublica and NPR spent several days with McKinney and fellow soldiers and veterans at Project Share, a charity to help brain-damaged soldiers. The program is based out of the Shepherd Center for Brain and Spinal Cord Injury in Atlanta, a nationally recognized hospital for head injuries.
Former Home Depot magnate and philanthropist Bernie Marcus founded Project Share in January 2008 to fill the gaps left by Tricare and military and veterans hospitals, which often lack the expertise and staffing to provide a full-scale program of cognitive rehabilitation therapy.
Cognitive rehabilitation is "very time consuming. It's not an easy deal," said Marcus. "Isn't this worthwhile? Isn't this something we should all be concerned about? Whatever it takes is what we should give them."
The visit revealed no flashy techniques, no cutting-edge medical devices. Instead, the men spent their entire days with therapists who focused on improving their memory, speech, balance and psychological health.
Soldiers got individualized treatment plans from a team of therapists who administered an intensive, two-week long evaluation to pin down their cognitive needs.
Therapists from different fields closely coordinated. A behavioral therapist provided counseling, since nearly all of the soldiers have post-traumatic stress disorder, a psychological injury which frequently accompanies traumatic brain injuries.
A speech therapist taught basic organizational techniques to overcome memory problems: How to make lists, how to pay bills, how to organize paperwork. A physical therapist helped them manage pain and relearn balance, which is often thrown off after a blast injury.
In the evenings, the men lived in apartments provided by the center. They did daily field trips, doing errands that are commonplace for most, but difficult for those with cognitive problems. They shopped at a grocery store. They cooked dinner. They helped assemble wheelchairs for the needy. They went to a horse park, where they combed, fed and rode horses.
At each step, a therapist helped them prepare for the job at hand. They suggested making to-do lists; using an iPod to keep track of medications; storing medical and military records into clearly labeled file folders.
Soldiers get a blue rubber bracelet with the initials SWAPS. The letters are supposed to remind them of a course of action should they become frustrated or mentally overloaded. The letters are an acronym: Stop; What's the problem?; Alternatives and options; Pick a plan; Satisfied?
The men stay for two and three months at a time. Afterwards, a Project Share worker follows them for up to a year to make sure that they are using the techniques they have learned to cope with life in the real world.
"It's very cozy and cocoon-like and warm and fuzzy here," said Tina Raziano, who visits soldiers and veterans at their homes and military bases to make sure they are adjusting. "When they leave here, they go through major, major changes. You really have to adjust to a new normal."
Cognitive therapy is not a silver bullet, nor is it a one-time treatment, or a rigid, well defined program. Instead, therapists here say, it employs a variety of techniques designed to do the hard work of retraining each soldier's brain to compensate for the things it can no longer do.
"We all see that they start out unable to do basic tasks," said Bonnie Schaude, a speech pathologist who coordinates many of the treatments. "People are leaving here, and they can function independently."
The visit made just as clear, however, the difficulty of implementing such an intensive, long-term plan for the military or Department of Veterans Affairs. Official Pentagon figures show that 188,000 soldiers have suffered some kind of brain injury since 2000. The number includes blast wounds, but also head trauma sustained in vehicle crashes, training accidents and household falls. Previous NPR and ProPublica stories have shown that the number likely falls short of the full tally by tens of thousands of soldiers.
The vast majority of head injuries are concussions, from which most soldiers recover quickly. The only treatment needed is bed rest and perhaps pain medication for headaches. But providing the kind of care available at Project Share to even the small percentage of brain-damaged soldiers who need it would require a tremendous commitment of time and money from military and veteran medical systems.
Project Share provides more than 30 hours of rehabilitation a week for several months at a time, and a year of follow up. In contrast, most VA and military systems can provide only a few hours of therapy a week. All Project Share's services are in one building, across the street from the Shepherd Center and its scores of cognitive experts. Military and VA facilities can spend months recruiting a single neurologist at a base for 30,000 soldiers.
The Pentagon's medical budget is $50 billion a year, expected to skyrocket to $65 billion by 2015. The system already cannot fill the slots available for psychologists, counselors and neuropsychologists, who can make better money in the private sector. The VA also has to care for an enormous population of aging veterans, whose geriatric needs are far different than the needs of injured Iraq and Afghanistan war veterans.
Project Share even has the resources to fly in family members and spouses on private planes, the costs and time donated by volunteers. A pilot flew Tiffany Dantzler, 22, from South Carolina to Georgia one recent day to visit her boyfriend, Ashley Craft, so the two could receive joint counseling on what to expect from brain damage recovery.
Craft, 26, sustained burns and a brain injury in a 2006 roadside bomb explosion in Iraq. After the explosion, he could not remember his own name. A specialist in the Marine Corps, he was medically retired in August 2007. He suffered from post-traumatic stress. He got angry quickly. A mechanic who worked on military vehicles, he could no longer tune up a car back home.
Craft got treatment at VA hospitals in Richmond and Columbia, S.C., near his home. But each time he left the programs, he felt lost and abandoned, he said.
His captain in the Marine Corps heard about Project Share, and got him admitted. Craft now hopes that the intensive rehabilitation will help him return to a normal life. At a recent session on anger management, he tried to take notes on a handheld memory device, painfully typing in one pointer after another.
"You're not the way you used to be. And it's really tough to grasp that concept," he said. "I used to think I was pretty good, and now I have to use a lot of adaptive equipment to remind myself, or to even be half as good as I used to be. That's what I got to do. That's my life now."
Shy and hesitant when he talks, a man who has seen his expectations dashed more than once, Craft said he is more hopeful, now. Project Share provides him far more intensive care than he was able to receive in the military, he said. His girlfriend has already noticed a difference.
"He seems more confident about what he says. His memory seems a little bit better," Dantzler said. "He seems more alive."
Marcus, the philanthropist who supports the program, said the expense and effort are worth it. In July 2008, he visited officials at the Army Surgeon General's office to pitch cooperation between Project Share and the military. He got a tepid response, according to Marcus and several others present at the meeting. The military said it wanted to focus more on improving its own treatment centers.
Marcus left frustrated. He had visions of an alliance between the military and a nationwide network of civilian treatment programs. Instead, Project Share has treated about 70 soldiers since it began two and half years ago. Since there's no formal relationship with the military, soldiers generally get referred by word of mouth. The military sent one therapist to receive training.
"That's where the problem is, trying to keep it internal when in fact you don't have the resources," Marcus said. "If you can't do it yourself, outsource what you can't do. That's the name of the game." Military and VA officials "all say things that you want them to say, but the bottom line is, it's not happening."
As he talked, Marcus grew agitated.
"I don't feel that Washington has paid attention to this thing. I don't think that Washington has done enough on this. I blame the president, I blame the Congress, for not giving these kids the opportunity to go on with a fruitful life after they have devoted their service to this country and put their lives on the line," Marcus said.
"It just doesn't make sense to me. It frustrates me. And it angers me. Kids are wandering around the streets today that will become tomorrow's criminals that were yesterday's heroes. How pathetic is that?
"We owe these kids a hell of a lot more."
Cpl. Brendan Jannesen, 23, a special forces soldier in the 75th Ranger Regiment, was patrolling at night in Afghanistan in August 2010 carrying heavy gear when he slipped off a trail, falling down a steep slope.
Tall, thin and fit, Jannesen had been a forward observer, trained to coordinate airplane and artillery strikes with soldiers on the ground attacking Taliban fighters. A math whiz, he could simultaneously juggle people screaming in both ears as he figured out the angle for incoming mortar strikes in the middle of battle.
When he awoke from his fall, however, Jannesen struggled to do simple arithmetic. He had to use his fingers to add. Jannesen's sergeant sent him to Project Share, hoping that its intensive approach would help.
Sitting in a common room with a poker table, Jannesen became passionate as he described how much he wants to return to duty, how much he has improved so far.
"I could do degrees, azimuth, you have to calculate the time of flight, the number of rounds, how fast your target is moving to try to get a direct hit on target. It was very, very heavy on cognitive demands," he said. "Now, I get worn out trying to write out a to-do list. It's very, very frustrating and very difficult to handle. You want to do stuff, but you can't do it."
About half the patients at Project Share are veterans, medically retired from the service and hoping to return to civilian life. The others are active duty soldiers who aim to return to their units. They are mostly Marines and special operations soldiers whose superiors have heard about the program through the close-knit communities that characterize those two forces.
Therapists say that nearly all of their patients are motivated: To get better, to navigate their lives, to recover from a baffling condition that has fundamentally changed the way they think and act in ways all but invisible to the outside world.
Mild traumatic brain injury "can be a blessing and a curse," said Irene Spychalla, case manager for Project Share. "These guys look completely healthy. They're walking, they're talking. You don't realize they're struggling with their daily lives."
A Marine since 1998, Sgt. Orville Wempner, Jr. was sitting on a tarmac in Iraq in 2004 when a mortar landed nearby. He remained conscious but was left with pounding headaches for weeks afterwards.
A water purification specialist, Wempner grew perplexed after he started having trouble operating the enormous, 5-ton pumping machine whose internal workings he had mastered long before the blast. He began to carry around a small green notebook to write down all his tasks. One day, he was alone taking care of his 6-year-old daughter and he simply forgot to feed her dinner.
Wempner, a Minnesotan known to his friends as Junior, knew that something was wrong. His brain, he said, was like a car engine with miswired spark plugs.
Wempner said his brain "feels like it's misfiring. There are days that I'm sitting there and everything is clear and then there's more days when I'm confused, not knowing what I'm supposed to be doing, where I need to go."
Wempner entered the Project Share program in September. Therapists worked hard on helping him learn to organize and prioritize. They retaught him to make lists. They trained him how to keep a calendar with all his appointments written down.
Basic stuff. But for Wempner, they were the tools to getting his brain working right again.
"It does sound pretty simple and down to earth," he said. "But when you're not thinking clear ... simple things like that don't really work."
For Brain-Injured Soldiers, Top Quality Care From a Philanthropist, not the Pentagon
Last month, the Pentagon sent a soothing letter to members of Congress worried about the treatment of soldiers who suffered brain injuries in Iraq and Afghanistan.
The letter, previously unreported, told House and Senate members that the military was studying the efficacy of a treatment known as cognitive rehabilitation therapy. Cognitive rehabilitation is a lengthy, often expensive program designed to retrain troops with brain injuries to do everyday tasks from remembering grocery lists to recalling words and names.
The letter includes contradictions of previous Pentagon statements. Notably, it makes no promise that brain-damaged soldiers will receive cognitive rehabilitation any time soon.
In the letter, George Peach Taylor Jr., the acting assistant defense secretary for health, acknowledged that the military health care's plan for troops and many veterans, called Tricare, does not cover cognitive rehabilitation therapy. One of the main reasons? A contractor hired by Tricare found limited evidence it works.
But as NPR and ProPublica reported Monday, Tricare's review came under fire in a series of confidential reviews by leading brain specialists. Scientists criticized the study as "deeply flawed" and "unacceptable." One even called it a "misuse" of science designed to hold down costs by depriving soldiers of care.
Cognitive rehabilitation has been used for decades to help civilians with brain injuries. Some major insurance companies, including Aetna and Humana, cover the treatment. Several major peer-reviewed studies support its efficacy. The Pentagon's own specialists and a panel convened more than a decade ago by the Institutes for Medicine have recommended its use.
Taylor's letter, which was written before the NPR and ProPublica stories appeared, did not mention the critiques of the Tricare study. But Taylor did make passing reference to another issue: money.
Comprehensive cognitive rehabilitation therapy can cost more than $50,000 per patient -- potentially adding enormous bills to the military's medical system at a time when hundreds of thousands of soldiers have suffered traumatic brain injuries on the battlefield. Tricare officials told us that money played no part in their considerations to deny coverage for the treatment. But Taylor told Congress that cost was a factor in figuring out which therapies to provide.
"Establishing the effectiveness of cognitive rehabilitation is an important issue for reimbursement of clinical services within the healthcare industry," he wrote to the chairs of the House and Senate Armed Services and Appropriations committees.
Taylor's letter also discussed a second set of studies, funded by $10 million set aside by the congressional committees in last year's defense bill. He wrote that the Pentagon's Defense and Veterans Brain Injury Center, known as DVBIC, had launched its own studies on how to treat mild traumatic brain injury. One of the signature wounds of the wars, mild traumatic brain injuries are often a result of blast waves from roadside bombs. Most soldiers recover quickly, but studies suggest as many as 15 percent go on to suffer lingering cognitive problems.
For careful readers of the military spending bills, this represents a significant change from what Congress had asked. The defense spending bill for 2010 asked the Pentagon to assess the value of cognitive rehabilitative in treating "traumatic brain injury in members and former members of the armed forces" (for those who want to read this passage in its full PDF context, you can check out the language on page 232 of the 1,236-page bill).
The difference is crucial. Why? Because cognitive rehabilitation therapy is actually a pretty well proven treatment for those suffering from moderate to severe brain injury. So by focusing only on mild traumatic brain injury, the Pentagon has avoided having to acknowledge the efficacy of the therapy for those with severe injuries, while tying up decisions on how to treat soldiers with mild traumatic brain injuries in a series of new studies.
In the letter, Taylor did say that cognitive therapy has proved promising: "Cognitive rehabilitation is a long-standing and significant component of comprehensive rehabilitation for individuals with moderate and severe TBI. There is an accelerating, but still small, body of scientific literature supporting cognitive rehabilitation in mTBI," he says, referring to mild traumatic brain injury.
Taylor said it will take years to complete the necessary studies. One should be finished in 2011, another in 2013. By then, many more troops will have suffered brain injuries. And many more who have already suffered blows to the head will have gone without cognitive rehabilitation therapy.
Why the delay? That's the question raised by soldiers, their families and brain injury advocates: if a treatment has some proof that it works, and no proof that it hurts, why not move faster to provide it?
"There should be a way to provide TRICARE coverage for cognitive therapy while further studies are ongoing," Sen. Mark Udall, D-Colo., who serves on the Senate Armed Services Committee, told us in a written statement. "We can't ignore the fact that many studies and experts have determined that cognitive therapy is effective for brain injured patients and the fact that the Department of Veterans Affairs already recognizes its value."
Rep. Bill Pascrell, D-N.J., co-chair of the Congressional Brain Injury Task Force, promised to send a letter to the Pentagon protesting its slow progress on cognitive rehabilitation therapy.
"It's unfortunate that this kind of foot-dragging has been what many have come to expect from the Pentagon when it comes to soldiers who have sustained traumatic brain injuries," Pascrell told us. "Brave Americans who risked everything for their country and sustained traumatic brain injuries -- the signature injury of the wars in Iraq and Afghanistan -- deserve cognitive rehabilitation therapy to help them secure the best futures possible. It is unacceptable that the United States has been at war for nearly a decade and there is still no plan to treat these soldiers."