Private Battles
On the road ahead, a turkey vulture lurches into the air. Mike Nashif, driving at a 60-mph clip with an 18-wheeler bearing down in the oncoming lane, realizes that a collision with the bird is unavoidable. His girlfriend, Anndra Mulholland, shuts her eyes and covers her face with her arms.
As if in slow motion, Mike sees the vulture hurtle toward him. He sees it hit the windshield and explode. He sees the web of cracked glass smeared with blood and feathers.
He slams the brake and swerves to the side of the road. He stumbles to the shoulder, swallows deep gulps of air and sinks to his knees with a groan. As he crouches by the side of the road, Anndra rubs his neck and back, saying: "It's OK, we'll be all right."
Mike, a two-tour Iraq war Army veteran, checks the car. It looks like it's been hit by a rocket-propelled grenade. A direct hit, too.
The collateral damage to his psyche will prove far more difficult to measure.
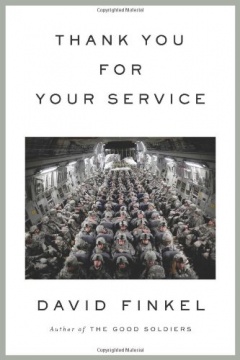
In April, after eight years in the Army based at Fort Hood, Texas, Mike took early retirement for medical reasons. He spent 27 months in Iraq dodging roadside bombs, rocket-propelled grenades, mortars and snipers. He saw friends die.
Army doctors noted his searing migraines, frequent nightmares, memory lapses, hyper-vigilance and anxiety. They diagnosed severe post-traumatic stress disorder and traumatic brain injury and recommended him for medical retirement.
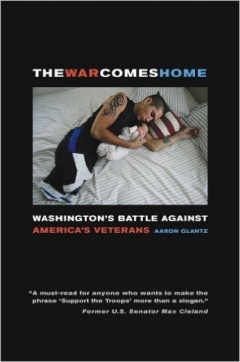
He lost much more than a military career. His marriage of 12 years fell apart, and he saw his four kids only every other weekend.
Experts say that there are hundreds of thousands of veterans like Mike. That PTSD is a dangerous enemy that destroys relationships. That families of veterans with PTSD often suffer deep psychological trauma, too.
After learning how to survive in the world's most hostile environment, Mike's mission these days is to relearn how to survive as a civilian.
Fishing is one of the few activities that helps Mike relax. That's why he and Anndra, the woman he's been seeing for about a year, spent a few quiet days at a lakeside retreat before heading back home to Belton, near Fort Hood. Driving through southeast Texas, Mike had felt calm in his Honda Passport, rolling past wide-open ranches dotted with broad-limbed live oaks.
But now, as he kneels by the side of the road, inspecting the damage caused by the turkey vulture, it occurs to him that life has just fired another lesson at him.
And it's knocked him to his knees.
Married with kids
In 2001, Mike was 24 and married with two children and one on the way. He'd met his wife, Dena, in Oregon, where they'd grown up. They'd moved to Texas to be close to Dena's mother in Waxahachie. Before enlisting, Mike had worked as an assistant manager at a grocery store, making $12.50 an hour. He was ready for a change.
In boot camp, Mike's drill instructor repeatedly harped on how soldiers needed to train hard because the world could change in a split second. Sure enough, Mike's graduation took place on Sept. 12, 2001, as the nation reeled from the terrorist attacks the day before in New York, Washington, D.C., and Pennsylvania.
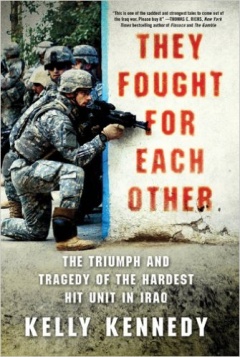
Just over two years later, in March 2004, Mike deployed from Fort Hood for a year in Iraq. He was one of the forward observers, who scouted enemy targets. Their base was in the volatile southern Baghdad sector. His 12-month tour of duty coincided with the heaviest fighting in Iraq since the initial invasion. Insurgents attacked troops with hit-and-run tactics. They ambushed convoys of Humvees and Bradley Fighting Vehicles with roadside bombs, or what the Army calls improvised explosive devices (IEDs).
On nightly missions, Mike would be either in the Bradley or a Humvee in a squad of three vehicles. The missions included patrolling hostile neighborhoods, checking houses for weapons or enemy combatants, and rebuilding roads and schools.
They were repeatedly exposed to roadside bombs. "I think my traumatic brain injury came from the repeated explosions. At least once a week, we were being hit by something," Mike says. "I think I had about 30 IEDs go off next to my vehicle, or within 25 yards of my vehicle."
One of them was a 250-pound bomb rigged to blow up in a parked car as he rolled by in his Bradley. Mike says he never heard the blast.
"You feel it, you smell it and you taste it," he says. "It's one big beat on your body. It's like somebody slapping you very hard on both sides of your body. You feel it on your toes, chest, head, fingers - all over your body."
Luckily, no one was seriously injured. Mike received a Purple Heart for shrapnel wounds on his hands and wrists, but it could have been worse. He found a piece of shrapnel embedded in the Bradley's hatch.
"A few inches closer," Mike says, "and it would have taken off my head."
During his tour, three close friends in his unit died. One was a medic who was sent home with a gunshot wound in his foot. He asked to rejoin his buddies in Iraq and was back less than a month when he was killed by an IED.
When another friend was killed by an IED, it was Mike's job to clean the shattered Humvee, removing blood and tissue from the electronics and radio gear that needed to be salvaged. "It took four hours to clean the blood out of the Humvee," he says.
Halfway through his tour, he faced perhaps his most traumatic moment: He was riding in the back of a three-vehicle convoy when the patrol was hit by a roadside bomb, mortars and gunfire. One of his closest friends, Spc. Raymond White, was killed in the attack.
Mike learned to become hard and leave his feelings behind whenever he went "outside the wire," military jargon for leaving the relative safety of the base.
"Everywhere you go, people are trying to kill you. You learn not trust anyone," he says.
War at home
When Mike returned home in March 2005, his wife noticed right away how much he had changed.
"He pretty much distanced himself to the point that whatever I did while he was gone, I continued to do," Dena says. "The bills, the children, the schooling, the doctors' appointments ... anything that needed to be taken care of here, I did."
At the time, Mike and Dena had three children, ages 4 to 10, and Dena was pregnant with their fourth child. Mike was scheduled to return to Iraq within 12 to 18 months. That didn't give him enough time to re-engage in the lives of his children, only to pull away again.
"It was like I was standing outside my house, watching my family through a window," he says.
When he did become emotional, he went off like a rocket. Mike admits he struggled with his short temper. "It was hard to control when I came back [from Iraq]," he says. "I went from zero to 90 in a half-second."
In a house with kids and dogs, the chaos and noise could be overwhelming. Once, when Mike's oldest son wouldn't stop poking his brother with a toy, Mike exploded in a flash. "I grabbed him by his throat and held him up against the wall," he says.
When one of the boys broke a wooden airplane model that belonged to his sister, Mike ordered his son to bring his favorite monster truck into the living room. Then Mike picked up a baseball bat and smashed the toy to bits.
In a war zone, instant obedience can save lives; disobedience is tantamount to mutiny. However, Mike could not distinguish between the battlefield and his living room. "My own anger scared me," he says.
He was having other problems, too. During a family road trip to Oregon to see Mike's father, Dena noticed that whenever Mike drove under a highway overpass, he would clench the steering wheel and open his mouth. In Iraq, insurgents would use overpasses to ambush convoys.
"I had to rub his arm and tell him he was OK. There were no insurgents, no bombs," Dena says.
He also struggled with searing migraines and bouts of dizziness and nausea - signs of possible traumatic brain injury.
Seeking professional help, Mike says, "was out of the question. He didn't want the Army to know he had psychological problems, "especially when your livelihood depends on your being promoted," he says.
He sought out his own forms of therapy. He began to spend a lot of time at fishing holes. "I had a hard time doing just about anything in public except for fishing," Mike says.
In many ways, he was still living as though he were deployed - putting up emotional walls and doing things that recreated the adrenaline rush he'd felt in a war zone.
While in Iraq, Mike had spent some spare time in Internet chat rooms, talking to women. For a soldier deployed thousands of miles from home, even virtual relationships could provide an outlet from the grinding tedium of life in Iraq. But one of those connections eventually led to an affair. Dena found out a few months after Mike deployed on his second tour in 2006. She was devastated. They quarreled during phone calls for the first three months of his deployment. Then Mike stopped calling.
"He pretty much told me he wasn't coming home," Dena says. "He didn't want to be a dad or a husband anymore."
Mike said he quit calling home because he felt helpless to fix his marital problems and he needed to stay focused on his mission in the war zone. When his second deployment ended in 2007, he and Dena had decided to make one last effort to save their marriage. They talked to a chaplain. They went on a marriage retreat. "It was kind of touch and go," Dena says, but at least they were living under the same roof.
About this time, Mike was put in charge of the recreation program for Fort Hood's Warrior Transition Brigade, a unit of soldiers trained to provide medical and other forms of support to wounded service members. Mike arranged fishing events in what would grow to become Take a Soldier Fishing, the nonprofit organization he runs today.
As he got to know wounded soldiers, Mike began to pay closer attention to his own medical problems. He suffered chronic headaches. He slept fitfully and suffered from nightmares. He hated crowded places - he wouldn't shop at Walmart and avoided busy restaurants. He met soldiers with similar symptoms, who were receiving treatment for post-traumatic stress disorder and traumatic brain injury. Eventually, he asked for help, too.
Meanwhile, he and Dena were working together to organize fishing events. But then came one final blow to the marriage. About mid-summer in 2009, Mike told his therapist about a dream he couldn't put out of his mind. In the vision, he saw his wife lying dead in the shower. He found the image disturbing enough to bring up in therapy.
Mike wasn't prepared for what happened next. He was immediately admitted to Fort Hood's psychiatric ward for five days of observation. He says he was put there because his dream was considered a "homicidal ideation." Mike vehemently disagreed and called his confinement a huge overreaction. Eventually, he and his therapist talked again and Mike concluded that his dream probably represented the death of his marriage.
Dena says Mike's dream extinguished any hope she had for their relationship. They agreed to divorce.
Mike said they tried for almost two years to fix their marriage. "I was living with my wife and kids, trying to do the right thing," he says. "But what I thought was right and what I felt was right were two different things.
"I know it's right to stay with your wife and kids and to provide for the family. At the same time, I needed to stop worrying about everybody else and worry about me."
At a crossroads
He met Anndra when he was at a crossroads, shortly after he was discharged from his short stint on the psychiatric ward. Weary and dejected about his future, a shadow of his former vibrant self, he was living out of a duffel bag in the Army barracks. He felt frozen in place, unable to go back to the way he had lived and afraid to leap forward into the unknown.
He responded to a long and quirky personal ad from Anndra; she said she liked guys with a mischievous sense of humor. That's how Mike used to think of himself: playful and impish. They arranged to meet - and immediately connected.
Anndra empathized with Mike's PTSD. Her first husband, a Navy veteran, had suffered a massive seizure and died suddenly in her arms, when she was 21. She lost her dad when she was 25 and her mother at 28. A mother of three young boys, she felt emotionally blocked and empty.
"Within the first week of seeing her, she knew everything there was to know about me," Mike says.
Over the last year, Mike and Anndra have been living together in Belton with her sons. But they plan to move soon to Lake Sam Rayburn in East Texas. The owner of a campground in Broaddus has donated a mobile home to use as the headquarters for Take A Soldier Fishing. Mike and Anndra are cleaning it up and planning to move in with her children this fall.
Anndra is learning to deal with Mike's PTSD. Whenever the artillery range at Fort Hood is in use, the sound of cannon booming makes Mike jumpy, she says. At such times, she scratches his head and rubs his neck and shoulders.
Safe and relaxing forms of recreation, like fishing, can provide an antidote to soldiers returning from war. That's one reason Mike decided to continue running his organization after leaving the Army. It's also good for his own therapy. "Take a Soldier Fishing gives a purpose to my life," he says.
He hopes the fishing events will create stronger family bonds. During previous fishing events, wives have seen their husbands open up with other vets about the war in ways they couldn't around their own families.
"I've had spouses come up to us and say, 'I learned more in 30 minutes of listening to them war-storying than I did in two years of asking questions,' " Mike says.
He thinks a program like this might have helped him. "If I had a program like this when I came back from deployment, I might still be married," he says.
But Mike's life has always been about change. Relearning to live as a civilian won't be easy. He knows there will be setbacks - like when a turkey vulture comes out of nowhere and ruins a perfectly good trip.
That day, Mike and Anndra climbed back in their car and continued driving home. Mike spent the next 50 miles feeling tense, white-knuckling the steering wheel and straining to see through the cracked windshield. He prayed it wouldn't rain and honked the horn to scare away any critters lurking by the side of the road.
But Iraq taught Mike that there's only so much you can control. That life can change in a split second. At times, that knowledge fills him with dread, and at other times, a kind of serenity.
"For me," he says, "the grass is a little greener, the trees are a little taller and the water's a lot prettier, just knowing it can be gone in a flash."
Some veterans get mental health help, but needs are far from being met
Two summers ago, Alexander Onzures was an Army medic assigned to a bomb removal squad in Afghanistan. The mission was to clear roads of improvised explosive devices.
"We had a saying," says Onzures, 24. "Sometimes we find them, and sometimes they find us."
Onzures was in Afghanistan only a month when an IED found his team. The explosion killed one soldier and wounded four others, including Onzures. Temporarily blinded, his back severely injured, he spent months recovering from his injuries.
In the meantime, four friends he'd lived with in Afghanistan were killed by another roadside bomb. By the time Onzures returned to Fort Hood, Texas, he was dealing with full-blown, untreated post-traumatic stress disorder.
"I was very withdrawn," he says. "If I was at work, then I was in a corner by myself. If I was at home, I was in my room, doors locked, lights off."
He tried to numb his physical and emotional pain, taking a daily dose of painkillers prescribed for his back and drinking half a bottle of Jack Daniels every night. Finally, a friend and fellow soldier suggested he enroll in a special program for soldiers with PTSD called Warrior Combat Stress Reset Center.
"He knew I was hurting," Onzures says. "He was a very good friend."
Opened in August 2008, the three-week program focuses on one of the core problems of PTSD - hyper-arousal, a state of mind that feels like a "stuck fire alarm," in which every situation seems to pose a threat, says Jerry Wesch, a clinical psychologist with the Fort Hood program. Hyper-arousal leads to avoidance behavior and social isolation, he says. Treatment combines traditional and alternative therapies, including counseling, biofeedback, breathing exercises, yoga and acupuncture.
Onzures' case had a positive outcome. But the military still says it falls short of meeting the mental health needs of all active-duty soldiers and veterans who need help.
Even Fort Hood, the country's largest base with 50,000 soldiers, is scrambling to meet the demand for services. Though Fort Hood offers a broad range of mental health services, it still must rely on local hospitals in Central Texas, such as Scott & White Healthcare, as well as independent therapists, to meet the needs of its military community, which includes more than 100,000 family members.
"We are not able to serve the entire population. So we are relying on our partners in the community to help provide some of that care," says Dr. Adam Borah, chief of Fort Hood's Resiliency and Restoration Center, which provides on-base outpatient mental health services. "We're lucky we have a relatively speaking robust network of community providers we can rely upon."
Nearly 20 percent of all combat veterans from the Iraq and Afghanistan wars - about 360,000 in all - report symptoms of PTSD and depression. Yet only a little over half of those have sought treatment, according to a study by Rand Corp. Many cite the stigma attached to mental illness for not seeking treatment, saying that doing so might harm their careers.
At Fort Hood, the number of soldiers diagnosed with PTSD has more than doubled - from 1,006 in 2007 to 2,390 through May of this year, according to the Carl R. Darnall Army Medical Center. In recent years, Fort Hood has hired more therapists to try to meet the demands for mental health services and make it easier for soldiers to find help. In January 2007, the Resiliency and Restoration Center had about 80 mental health specialists. As of July 2010, that number had doubled to 161 A year ago, Fort Hood opened a new resiliency center, a one-stop wellness hub. The sprawling campus houses a gym and meeting rooms with a choice of services, including licensed mental health therapists, chaplains, massage and acupuncture.
Increasing numbers of war veterans are leaving active-duty service and returning to their communities. There are 12,038 Iraq and Afghanistan war veterans enrolled in the VA North Texas Health Care System. Various programs, both public and private, are reaching out to them and others who are not yet in the system.
The local VA recently expanded services for recent combat veterans. New community-based clinics have opened in Mesquite , Arlington, Fort Worth and Far North Dallas to supplement services offered by the Dallas VA Medical Center in southeast Dallas.
The VA also has begun offering special classes for spouses and other family members. "When you're dealing with readjustment issues, the role of the family has unfortunately been downplayed in the past," says Michael Heninger, a licensed clinical social worker at the Vet Center in Arlington.
"We are here for families of war-zone veterans," offering classes and services at no cost, Heninger says. "They've already paid the price."
Soldiers' survival rates on rise, but so are challenges presented by brain injuries
Thanks to advances in combat gear and battlefield medicine, more troops survive injuries that would have killed them in previous wars.
This is good news, but it also presents some long-term challenges. The soldiers are "surviving, but with things like post-traumatic stress disorder and traumatic brain injury ," said Dr. Carol Tamminga, professor of psychiatry at UT Southwestern Medical Center.
Traumatic brain injury, or TBI, is caused by a blow or jolt to the head, or a penetrating head wound, that disrupts the function of the brain. Because of its prevalence, TBI has been called one of the "signature injuries" of today's wars, along with PTSD.
An estimated 19 percent of the 1.8 million troops who have served in Iraq or Afghanistan - about 342,000 - may have experienced a traumatic brain injury during deployment, according to Rand Corp., a California-based nonprofit research organization.
More than half of those cases, however, go undiagnosed and untreated, the Rand study said. The reasons: There is no simple check, such as a blood test, to diagnose TBI, and many soldiers do not seek treatment for concussions.
About 75 percent of all injuries to troops in Iraq and Afghanistan have been caused by blasts, including roadside bombs. Only the most severe head injuries are visible. Most head injuries remain hidden inside the skull. Symptoms of the more common mild TBI can include headaches; dizziness; temporary loss of balance and memory; insomnia; and depression.
Researchers don't completely understand TBI's long-term health effects. One of the problems is that TBI's symptoms are so general, they "can be associated with something serious or not so serious," said Tamminga, who served on an Institute of Medicine panel examining TBI.
The TBI panel looked at previous studies that didn't include soldiers in the current wars. The panel found that those who suffered moderate or severe brain injury were more likely to have dementia, Parkinson's disease, diabetes and PTSD.
But the panelists cautioned that there has been no comprehensive review of head injuries from the Iraq and Afghanistan wars. They recommended that the Defense Department and the Department of Veterans Affairs conduct such research as soon as possible.
In Texas, Fort Hood's TBI clinic has seen 3,081 patients since opening in November 2008. "What we don't know is how many of those are simple screenings, and how many needed follow-up [care]," said Heath Steele, spokesman for the Carl R. Darnall Army Medical Center.
PTSD and TBI are separate conditions but can go hand in hand. While PTSD can be caused by a brain injury, it "can be associated with any kind of stressful, life-threatening experience, not necessarily TBI," Tamminga said.
TBI and PTSD are "associated with traumatic memories and traumatic situations. These memories are seared into the mind ... almost permanently implanted. So the treatment is really long term," Tamminga said. "You can give pills to help people sleep, and pills that decrease anxiety. But you can't give pills that cure troubling memories. You have to really work through with the person those troubling memories."
Doctors can work through disturbing memories in a professional way, Tamminga said, but families also can play a role.
"Patience and understanding will do an awful lot to support people as they go through this process," she said.
- Previous Section
Private Battles - Next Section
An Unexpected Enemy