While the debate is focused on the power of naming a disorder, it really represents a far more important set of nuanced issues and assumptions about the nature of psychological responses after surviving catastrophe, brutal deaths, war, sexual assault and other horrific life events. It also represents differing views on how best to achieve needed cultural changes.
For reporters covering this debate as it unfolds over the coming months – whether about veterans, public health, science or policy – it is crucial to understand that there are many points of agreement among these contending experts. Most fundamentally, both sides are deeply committed to remedy any long-standing problems that survivors face after confronting a traumatic event. While the debate about the APA diagnosis rages on, it’s important that the media and the public do not lose sight of just how much agreement there is among mental health professionals when it comes to trauma and PTSD:
There is clear agreement about a defined set of enduring symptoms and problems that some, but not all, survivors experience long after an overwhelming, traumatic event that creates problems in functioning. There is agreement on real changes in emotions, behavior, thoughts and brain functioning. There is no question that we’re talking about a real psychiatric condition, that the diagnoses represent a clear set of empirically determined symptoms, and that the APA needs to specify this condition. There is no debate that a condition exists; that trauma-related problems occur on a continuum; some people have functional impairments (i.e. disorders); and others have trauma-related distress (an array of injuries). All require different interventions. We agree that we need to leverage natural healing processes, social support, culturally acceptable formats, and individual strengths. And we all agree that not all trauma-related pain is in fact a disorder.
All parties to this PTSD/PTSI argument want to remedy a very alarming reality – although we have effective psychological and pharmacological solutions to help survivors who are struggling, many survivors do not access – or cannot access – these effective services for a variety of reasons. As documented in a new report from the National Institutes of Medicine, barriers to care, for military members and others, are substantial.
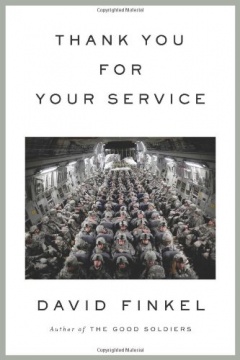
- Clearly those in the service still worry about the impact of having a PTSD diagnosis might have on their military career. Those in the military, and elsewhere, may avoid treatment since they don’t want to suffer prejudice or discrimination for having a mental disorder. In a culture that teaches soldiers to handle whatever challenges confront them, any vulnerability may be seen as shameful. Perhaps sufferers don’t recognize that they have a problem – whatever its label. Perhaps they don’t believe useful remedies exist. Perhaps our remedies are not in the format that survivors need. Perhaps avoidance, a key aspect of PTSD, prevents them from seeking help. Perhaps the structure of health delivery is not working and needs to be changed. Perhaps a key aspect of coping, minimization and denial, prevents them from labeling trouble. Yet the fact is that people are not getting the help they need even when it exists. It is troubling for all of us.
- We all agree that the military and other organizations that put people in harm’s way and increase a person’s occupational risk of developing PTSD have a responsibility to address it. This means reducing risk of developing PTSD and providing access to services addressing PTSD when it occurs. This requires changing every possible barrier for accessing help and improving the culture of the recovery environment, and is a challenge that will exist whether this signature psychic wound is labeled PTSD or PTSI. Military cultures, and many other occupational cultures as well, need to establish not only new policies and procedures but new cultural norms about trauma exposure and its effects.
- Addressing psychological outcomes as a result of an occupational hazard, should be not seen as a weakness, but an act of courage and a means of performance optimization. This may include classifying PTSD as an occupational stress injury within the military system, providing parity for both physical and mental health causalities of war both in recognition and medical care, and changing and providing new models of care delivery.
- We also all agree that globally the culture needs to change when it comes to trauma (and mental health in general). We need to cease blaming victims. We need to challenge ways that society creates, maintains and worsens problems for survivors. Certainly some catastrophic events are acts of nature, but many traumatic events are caused, and/or worsened, by social conditions – patriarchy, human rights violations, unfair systems, organizational structures, political mistakes and the list goes on. We need to mitigate risks, reduce stigma, and actively change our environment. We need to facilitate a culture where survivors’ recovery is honored. We need to instill connectedness among survivors and non-survivors in our culture. Among trauma experts there is no disagreement here.
- Interestingly, the debate about renaming PTSD represents two common and differing strategies in the field of traumatic stress studies. The field of traumatic stress was borne of—and continues to be enhanced by—one of those strategies: the pursuit of social justice, actively acknowledging, opposing, challenging and changing the social conditions of those who suffer from violations, indignities and oppression. Thus the grassroots campaign to change the diagnostic label from Post Traumatic Stress Disorder to Post Traumatic Stress Injury represents a very important product of social activism and victim advocacy.
The process of engaging scholars, policy makers, clinicians, and survivors equally to advocate for change is arguably a healthy, much needed effort to use scientific terminology to reduce stigma and effect social change. It’s had honorable precedents: In the past, successful grassroots campaigns for the DSM revisions involved changing or considering pejorative language describing proposed disorders – diagnosIs such as masochistic or self-defeating personality disorder, (not surprisingly these were to be applied to women suffering from sustained interpersonal violence) or disorders that were not yet clearly evidence-based (Pre-Menstrual Dysphoric Disorder).
This time around, advocates for the PTSI label are arguing over the term “disorder” itself: The notion here is not that the disorder does not exist, not that the DSM process is faulty, nor that PTS is pejorative in and of itself, but that “disorder” needs to be changed, that language is both symbol and engine for changing social attitudes toward survivors of violence.
The alternative strategy – which has also fostered dramatic improvements in the lives of victims – is the use of scientific evidence. We have so much clear scientific knowledge about the phenomenology, assessment and treatment of PTSD that has aided survivors in the mere thirty-two years since the diagnosis was placed in the DSM. While science is certainly affected by political decisions – by funding, by political priorities, by economics – (science primarily uses evidence to determine next steps. Science may be imperfect, conservative and slow, but changes in science occur through the repeated amassing of quality evidence to inform social policy. My observations from the outside of the APA DSM-V PTSD committee is that the members have been very willing to entertain many ideas, but have been quite vigilant about only recommending changes based on clear, peer-reviewed, high-quality evidence to support those arguments.
I have searched and found no hard evidence that a name change will help reduce stigma. The name “schizophrenia” does not have “disorder” in it, yet it is a highly stigmatized disorder. In other words – when it comes to PTSD, more evidence needs to be provided to demonstrate that the name change will reduce stigma.
And yet a grassroots campaign to change the name of a scientific diagnosis represents what I most love about this field – the recognition that both science and politics are involved in rectifying trauma. I find it inspiring that professionals involved in the DSM-V revisions are even willing to engage in this conversation at all about the word “disorder” – after all the DSM-V is a short for the Diagnostic and Statistical Manual of Mental Disorders. The engagement of activists and scientists on this issue represents the true essence of the field of traumatic stress – and that’s what journalists need to understand. In 1980, we were fighting – politically – to have the PTSD diagnosis recognized – scientifically. Yet here we are in 2012 together discussing the issues of which should come first – politics or science.
The trauma field recognizes the need to address the problems at all levels – social advocacy, scientific knowledge, policy changing, changing cultural norms, political organizing. We must enact policies to reduce violence in civilian life, mitigate the effects of war on soldiers and civilians alike, and limit disaster’s devastation. We need to hone scholarship about PTSD stigma, barriers to care, and evaluate public education campaigns and enact changes based on this.
Together, using many approaches, we can help survivors. But focusing on a diagnostic label is really not the core issue. Changing conditions related to trauma, changing health care access, and changing societal attitudes about traumatic events and the aftermath – on that, all sides align.