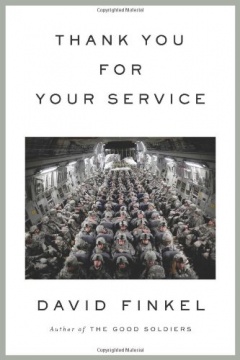
'Unprecedented' Report Examines War Effects
About one out of six veterans (15.6 to 17.1 percent) returning from Iraq met criteria for combat-related psychiatric disorders, including depression and Post-Traumatic Stress Disorder, researchers say in a report published today in The New England Journal of Medicine.
About one out of six veterans (15.6 to 17.1 percent) returning from Iraq met criteria for combat-related psychiatric disorders, including depression and Post-Traumatic Stress Disorder, researchers say in a report published today in The New England Journal of Medicine.
The study, conducted by the Walter Reed Army Institute of Research, and led by Charles W. Hoge, surveyed soldiers before and after deployment in Iraq and Afghanistan. In an editorial also published today in The New England Journal of Medicine, Matthew J. Friedman, executive director of the National Center for PTSD, a division of the Department of Veterans Affairs, called the study "unprecedented." Previous studies of the effects of combat on mental health were conducted years — and sometimes decades — after soldiers and marines had returned from battle. "This is the first time there has been such an early assessment of the prevalence of war-related psychiatric disorders, reported while the fighting continues," Friedman writes.
Researchers found that only 38 to 45 percent of those who met criteria for a mental disorder were interested in receiving help, the report said. "And only 23 to 40 percent reported having received professional help in the past year." The study found that soldiers and Marines who met criteria for a mental disorder were twice as likely to report negative feelings about seeking mental health services.
- 41 percent said seeking care "would be too embarrassing."
- 50 percent said it "would harm my career."
- 59 percent said: "Members of my unit might have less confidence in me."
- 63 percent said: "My unit leadership might treat me differently."
- 51 percent said: "My leaders would blame me for the problem."
- 65 percent said seeking mental health services would cause them to "be seen as weak."
About 12 percent of troops returning from Iraq met the strict definition of PTSD. For comparison, according to the report, "rates of PTSD among the general adult population in the United States are 3 to 4 percent." In a study conducted in the mid-1980s, about 15 percent of Vietnam veterans met PTSD criteria. A study conducted between 1995 and 1997 found a PTSD rate of 10 percent among Gulf War-era veterans who had experienced combat duty. However, another study of veterans of the first Gulf War found that the prevalence of PTSD more than doubled two years after their return from combat.
The study found a linear relationship between the number of firefights during deployment in Iraq and the prevalence of PTSD:
- 4.5 percent for no firefights
- 9.3 percent for one to two firefights
- 12.7 percent for three to five firefights
- 19.3 percent for more than five firefights
In his editorial, Friedman said it is possible that the reported prevalence of PTSD may increase in coming years. First, he noted the study of Gulf War veterans that showed that "the prevalence of PTSD may increase considerably during the two years after veterans return from combat duty." Second, he writes, "it is possible that psychiatric disorders will increase now that the conduct of war has shifted from a campaign for liberation to an ongoing armed conflict with dissident combatants." (The study participants were surveyed three to four months after their return from combat duty; troops who served in Iraq during the past few months of increased fighting with insurgents are not included in the study.) "It may simply be too early to assess the eventual magnitude of the mental health problems related to deployment to Operation Iraqi Freedom or Operation Enduring Freedom," Friedman writes.
Despite this, Friedman sees many hopeful signs that today's veterans may fare better than those of previous eras. "Collaboration between mental health professionals in the Department of Defense and those in the Department of Veterans Affairs is at an all-time high," he writes. And he notes several other factors:
- Public support for returning soldiers appears to be strong, "despite sharp political disagreement about the war itself," he writes.
- "Study of PTSD has matured to the point where effective evidence-based treatment and practice guidelines are available for use by the Departments of Defense and Veterans Affairs and by civilian mental health practitioners."
- "Cognitive-behavioral therapies have been successful in the treatment of PTSD, and two selective serotonin-reuptake inhibitors have been approved by the Food and Drug Administration."
However, Friedman and the researchers stress the need for improved monitoring of veterans' mental health after their return from combat as well as the need to ease the stigma associated with mental health disorders.