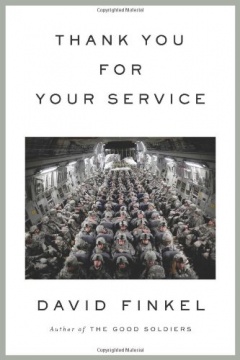
At War: Notes From the Front Lines
Brennan, who suffered a traumatic brain injury in Afghanistan and was diagnosed with PTSD upon returning home, offers a uniquely personal and clear-eyed account of military culture and life as a veteran. Judges called Brennan’s blogging “fresh,” “powerful” and “profound.” Brennan's contributions to the "At War" blog were originally published in the New York Times in 2012.

LIVING WITH P.T.S.D. AND ALLOWING MYSELF TO GET HELP
BY THOMAS BRENNAN
An alarm clock chimes across a pitch-black room. I slowly rise. Standing in my bathroom, I brush my teeth and shave away yesterday’s stubble – part of every Marine’s mandatory morning routine. The person in the mirror seems somehow unfamiliar. Downstairs, the morning pot of coffee brews. I finally begin to wake. Leaving home, the roads are lined with beautiful farmland, backlit by a rising sun. Morning dew glinting off the fields gives way to a kaleidoscope of neon signs as I reach town. Pulling into the parking lot, I take a deep breath and step out of my truck.
Driving home, I am greeted by the sun as it sets across the farmland. I park my truck and then open the door to my house. Unbuttoning my uniform and slowly taking it off, the facade I wore all day fades away and relief washes over me. “Daddy, Daddy, you’re home!” my daughter yells. Most parents feel a sensation of happiness when greeted by their children. At this moment I am sad, empty. I give her a hug, but she feels far away. I lie on the couch, feeling lost.
There are 1.7 million Veterans from Iraq and Afghanistan, and at least a third of them suffer from post-traumatic stress disorder, or P.T.S.D., according to the National Center for P.T.S.D.
I am one of them.
P.T.S.D. is an anxiety disorder that can occur after a traumatic event. Given that troops deployed to Afghanistan and Iraq see fallen comrades, experience combat, or survive horrific events, the likelihood of a veteran being diagnosed with P.T.S.D. is high. According to the Department of Veterans Affairs, someone with P.T.S.D. is at least twice as likely to commit or attempt suicide, or experience substance abuse. Tens of thousands, if not hundreds of thousands, are suffering from alcoholism and drug abuse, depression or mood disorders, according to a 2010 report by the Coalition for Iraq and Afghanistan Veterans.
The Center for a New American Security discusses the stigma in the service associated with mental health treatment. In a study on the rising suicide rate in the military, the organization found that troops were two to four times more interested in receiving care than reported but were afraid of repercussions from their superiors. That same fear initially kept me from getting treatment. But I finally sought help. My superiors met me with neither resistance nor support. It felt like I lost their respect, that they forgot who I was and what I had done for the Marine Corps during my tours in Iraq and Afghanistan.
P.T.S.D. is something that some in the military do not accept or understand. Unlike physical wounds, it is invisible, intangible. I once heard a senior Marine say P.T.S.D. was “fake.” In a way this makes sense for a military institution that prides itself on toughness and resilience in the face of adversity. But the time has come to realize that all battlefield wounds must be healed.
“While the military is making some steps to make it easier and more accepted to seek care there is still a long ways to go,” says Jason Hansman of Iraq and Afghanistan Veterans of America. “Even with top military officials coming out and saying they seek help that is still not enough to correct this stigma.”
Some 57 percent of those who suffered mental health problems on active duty received treatment in 2010, up from 36 percent in 2008, according to the Department of Defense. The department is slowly trying to remove the stigma associated with P.T.S.D., depression and mental health treatment.
But nearly a million disability claims are still delayed in processing, as reported by the Department of Veterans Affairs. Without a disability claim, veterans must pay out of pocket or use private health insurance for mental health treatment. There are reports of suicidal veterans being turned away because of lack of staff. When a veteran requests V.A. mental health treatment, he must be seen within 24 hours. This happens in most of the time, but follow-up appointments that should be completed within two weeks are often delayed nearly two months.
The countdown to returning home from deployment starts the moment you step foot on the bus to deploy. Arriving home to the daily grind, you wonder if it would have been easier to stay abroad. Overseas there is a sense of normalcy amid the chaos. Reconnecting with your family and revealing what you have become is often scarier than taking that next step on patrol.
I arrived home from deployment scared yet happy, excited yet terrified. I left when my daughter was 2 and returned when she was 3. I had deployed before but never as a father. When I left, she was completely dependent on me. Now it was, “I can do it myself, Daddy.” That depressed me. Stepping on the bus you expect time to stand still and things to be somewhat the same when you got home, but things change. One, two, threes turn into eight, nine, tens, and bath time turns into her taking her own showers. I would turn the water on for her and she would have me leave the room, closing the door behind me. The morning rituals had changed. She has begun to make her own breakfast, wanting to pour her own Cheerios and milk. She even started turning on the TV herself. The days of her sitting on my lap watching “Dora the Explorer” were over. I felt slightly abandoned. Of course she still came for me, just not the way she once did. Life as you once knew it drifts away, and the little girl you left behind seems all grown up.
Everywhere I traveled on deployment I brought a wall of my daughter’s artwork. I kept a picture of her in my pocket, but by the time I got home it barely resembled her.
There was more. I saw disturbed patches of dirt as threats – potential roadside bombs – loud noises made me jump and silence made me paranoid. Seven months in a combat zone makes it difficult to switch off. Multiple close calls with death made me feel like I should not be alive. I avoided contact with my wife and daughter. I went through the motions. Hugs and kisses felt hollow. Smiles had no feeling, tears bore no sadness. I had become so numb that I was just a shell of my former self. I often found myself lying on the couch, blankly staring at the television for unknown amounts of time. Survivor’s guilt was affecting me. I could not look at my legs without thinking of those who were still struggling through physical therapy or worse.
Unlike so many other families, mine was lucky. I came home. Not the same person, but I was home. I struggled daily. Images of what my wife would be like if I had died rushed through my head frequently. Life without me in it became my fascination. Daydreaming became my escape from reality. I would imagine my daughter riding her bike for the first time without me. Or my wife at the altar remarrying years later. I was physically present, yet mentally troubled with thoughts of my demise.
Every 24 hours a member of the military commits suicide. Every 80 minutes a veteran does the same. Nearly one in four suicides in this country is either a veteran or service member, yet we only make up 9 percent of the population according to the Census Bureau. High suicide rates are largely due to the isolation and hopelessness felt by many service members once they return home, according to Iraq and Afghanistan Veterans of America.
This plague in our military community is due partly to the lack of mental health providers in the V.A. system. In 2012 the department says it is planning to hire 1,600 new mental health professionals. But changes in manpower and policy will not occur overnight.
My change started slowly. Thankfully I did not lose any of the Marines in my squad on my most recent deployment, but four of us were wounded on an operation. Three were hit by an explosion from a rocket-propelled grenades and suffered traumatic brain Injuries. As the smoke from the explosion cleared, I looked them over; faces blackened with soot, their eyes dilated. We shared the same look of fear. I began maneuvering my men across the battlefield despite wanting to abort the mission. Minutes later, I was briefly knocked unconscious by a second explosion. I distinctly remember feeling failure as we were airlifted to Camp Bastion Air Field for treatment. On the medevac helicopter all I could think about were my Marines still on the ground. I imagined their resentment and disapproval of the decisions I had made that day. I would ask myself repeatedly whether they would ever trust me again.
The injuries reminded me of the people I had lost in the past. Suppressed emotions surfaced. As a leader I was strong, but as an individual I began to fall apart. The day I was injured shook me. I felt as though I was not the strong leader my men deserved. My Marines were wounded because of my decisions, and I have not forgiven myself for that. I hated going out on patrols after that day, because I feared another attack. Those Marines will never be the same because of me.
The traumatic brain injuries we suffered are the most prevalent injuries facing troops in the Middle East. They come from a blow, jolt or blast to the head. According to the Mayo Clinic, traumatic brain injury ranges from mild, with symptoms of short-term memory loss, mood swings, light sensitivity and sensory problems, to moderate, with symptoms of long-term memory loss, slurred speech, loss of coordination, and seizures, or to severe, which can resemble mental retardation. The Brain Injury Association of America estimates that more than 360,000 troops have suffered traumatic brain injuries since 2001, with many unreported cases. The Pentagon’s Defense and Veterans Brain Injury Center reports that approximately 30 percent of all casualties evacuated from Afghanistan and Iraq and treated at Walter Reed Army Medical Center had traumatic brain injuries.
Afghanistan changed me, and I knew it. I felt it before I got off the bus, and it worsened as time went on. It did not take long before the change began to show. My work and family relationships began to suffer. I became sluggish and depressed as my past caught up with me. For months, my daughter’s smile could pull me out of any funk, but eventually not even she could cure me. On Oct. 29 2011, seven months after I came home from my deployment, I began treatment.
Some wounds have healed. Others still have scabs. In order to fully heal I need to peel back those scabs to reveal what lies beneath. Therapy has revealed many weaknesses, but it has also highlighted my strengths. I have since forgiven myself for what happened on the day we were injured. I now feel when I cry. There is emotion behind my hugs and kisses. My past no longer haunts me.
*****

WRITING TO CALM AND COMPOSE THE INJURED BRAIN
BY THOMAS BRENNAN AND COBAN SHAW
Those men are gone.
There is an old “we” with the ability to multitask. We could recall anything after hearing it only one time. School was easy; lectures simple to understand and we could remember where we left things. We always won anything involving strategy. We remembered our wives and our anniversaries as well as our children’s birthdays.
Those men are also gone.
The two of us suffered traumatic brain injuries, one of us in 2006 in Iraq and the other in 2010 in Afghanistan.
Traumatic brain injury is defined as damage to the brain as a result of injury, often from a violent blow or jolt to the head. Since 2001, the military has confirmed traumatic brain injury in more than 220,000 of the 2.3 million troops who have served in Iraq and Afghanistan.
Post-traumatic stress disorder is an anxiety disorder that some people develop after seeing or living through a dangerous event. The independent Institute of Medicine reports that “an estimated 13 to 20 percent of U.S. service members who have fought in Iraq or Afghanistan since 2001” suffer from P.T.S.D. It has become the signature injury associated with the past decade of war.
Traumatic brain injury and P.T.S.D. have many overlapping effects. The National Center for P.T.S.D. states that symptoms include memory problems, depression, angry outbursts, focus issues and insomnia.
Often people associate a traumatic brain injury with a specific set of symptoms. But such injuries are unique to each person depending on what area of the brain was damaged in the blast or blow to the head. While we share similar symptoms, we have unique problems.
I’ve learned that some of us share one thing in common — a keyboard or a pen. They melt away our symptoms. Unlike spoken words, the individual letters flow into paragraphs effortlessly. Upon meeting we shared a long conversation discussing how, before our injuries, we struggled with writing, as we now struggle with speaking. The way our injuries have affected us are truly intriguing, and comical, at the same time.
We met in Washington, at a seminar known as the Veterans Writing Project in August. Immediately, we felt a bond, despite being surrounded by fifteen other veterans, with our injuries giving us common ground.
Founded by Ron Capps, the Veterans Writing Project provides no-cost seminars to train and encourage veterans and their family members to tell their stories. The program also focuses on using writing as a nonclinical approach to dealing with P.T.S.D. as well as traumatic brain injury.
Mr. Capps, a 25-year Army veteran who served in Afghanistan, Iraq, Rwanda, Kosovo and Sudan, was diagnosed with post-traumatic stress disorder. He was medically evacuated from his last deployment in 2006 after becoming suicidal and left service in 2008. When medication and talk therapy weren’t working, he turned to writing.
“I wrote myself out of a very dark place,” he says.
He founded the Veteran Writing Project in 2011, after attending the graduate writing program at Johns Hopkins University.
“All our instructors are working writers who are also combat veterans,” Mr. Capps says, “Our literary goals are to give away the skills we’ve learned to others in the hope they will tell their own stories.”
But beyond literary goals, there are others. All of the Veteran Writing Project instructors are also part of the National Endowment for the Arts’ Operation Homecoming, which provides expressive and creative writing instruction to service members at the National Intrepid Center of Excellence, a Defense Department research and treatment facility on the campus of Walter Reed National Military Medical Center.
“Writing allows us to shape and control traumatic memories,” Mr. Capps says. He goes on to say that through writing those who suffer can distance themselves from the trauma, introducing metaphor and narrative to what would otherwise be a re-living of a life or death moment – a flashback to when their brain and body were in fight or flight mode.
“Lots of people are skeptical that this works,” he says. “But there are 20 years of studies.”
And while it won’t be helpful for everyone, “Some of these guys are now writing as part of their individual recovery,” he adds.
The arts have been shown to be excellent forms of therapy for service members and veterans. There are many organizations promoting artistic healing and that claim outstanding results. Organizations such as They Drew Fire use drawing and now there is the Veteran Writing Project.
We both have used writing as therapy. Whether it’s outside with a steaming cup of coffee on a sunny Saturday morning or lying in bed plugging away at the keys, writing has been instrumental in quelling our inner demons and bringing a sense of normalcy to our lives. Countless hours have been spent recounting our experiences in theater, which has desensitized us to the traumas. Many more hours have been spent locked in the computer screens’ glare, tapping aimlessly with one goal. To feel normal once more.
There is a new “we.” Being able to tell our stories through writing has been instrumental in our therapy and facing reality. It has allowed us to cherish and accept our past rather than ignore it. Writing has eased the transition from old to new and we are now more hopeful of the future.
Because of writing, those men are here.
There is a new “we.” Writing enables us to make our thoughts and memories tangible so that we can remember them later. We can plan and organize our feelings to be successful as the new we. It provides us with a medium to express our thoughts and ideas so that we can communicate well with others.
*****

ENDING A life, and part of yourself, for the first time
BY THOMAS BRENNAN
I was scared, to say the least. It was the first time my training would be tested. I heard my rifle crack as I fired. The weapon’s recoil nudged my shoulder, and he crumpled to the ground. The aroma of gunpowder filled the room. I fired two more rounds into his motionless body, then stared in amazement as his body lay lifeless, his black and red scarf astray. The sun rose across the city’s skyline. I was 19.
For me, the 10th of November is special. It is the Marine Corps’s birthday, a day for celebrating camaraderie. But it is also the day, eight years ago, when I was pinned down in the relentless firefights of Operation Phantom Fury. It is the day when I took a person’s life for the first time.
These two drastically different events make for mixed emotions at that time of year. In 2004, fighting in a large-scale attack on the corps’s birthday was thrilling. I’d be lying if I said that I am not still motivated by the memory. What better way to celebrate 229 years of decorated service than to take part in writing the corps’s next chapter? But I also feel as though I lost a part of myself that day.
Taking someone’s life brings you to the darkest side of yourself. There are nights when I see the faces of people I killed. There are days when I get lost in vivid memories of violent combat for minutes at a time. But it also leaves you emotionally numb. In the last eight years, I have not been able to cry unless I am reminiscing about Falluja. It is as if my brain created a space where feelings were lost or delayed. And when I did feel emotions after killing, it was often the sense of relief that I was not on the receiving end – an emotion that might readily, but incorrectly, be interpreted as satisfaction.
It was easy then to fall back on the powerful logic that it was either me or them, or worse yet, one of my fellow Marines. But that logic leaves questions with no easy answers. Did I in some ways come to enjoy killing? Was the loss of a life, and my innocence, worth it?
Pulling the trigger for the first time was beyond difficult. But the more I had to do it, the easier it became. With each passing trigger pull I lost more and more of my innocence. In fact, I actually started to get used to “slaying bodies,” as we called killing the enemy back then. And as more and more of my comrades were injured or killed, the sweeter the revenge began to taste. Looking back on it now, I feel bad that I did not feel bad.
Taking someone’s life changes you whether you like to admit it or not. It took me a long time to notice and admit the changes in me. It is something most people will never have to do. I am envious of those people. I look back on taking an insurgent’s life and can’t help but think I went a little crazy from doing so. I wonder from time to time what I was like before that day many years ago. But I also realize I will never be that person again.
I cannot be alone. In the wake of a suicide epidemic among veterans and active-duty troops, there must be others dealing with these demons. There must be other combat veterans caught in a moral struggle over their wartime actions.
Despite pondering these thoughts for many years, I chose to re-enlist in 2006 knowing for sure that I would go to Afghanistan. Part of me wanted the rush that combat gave me. After being so close to death, things that once excited you have a way of losing their thrill when you return home. I wanted to feel alive again. Strangely, that involved surrounding myself with the threat of death.
Afghanistan was very different from Iraq. The Taliban were very persistent in recovering their wounded. My squad fired thousands of rounds, but the most we ever saw was blood spatter and entrails. No dead bodies. No proof that we killed anyone.
The firefights were intense. Some of them lasted hours. The enemy mastered complex ambushes and attacked us from multiple locations at once, which truly tested my leadership. The fear was real. The bullets were real. I loved it, and with time, my men did too.
At the beginning of our deployment to Afghanistan, I was the only one in my squad with combat experience. The first time we took fire, my men briefly froze, just as I did years earlier. Looking at their faces I could see the fear as they struggled to accept our reality. But within seconds of the first rounds’ hitting our position, their training kicked in and we not only suppressed but also maneuvered on the enemy. The pride I felt watching my men execute their training was immeasurable.
After our first encounter with the enemy I knew they had felt what I had felt, and wanted to feel again. It was all they talked about. And when we went for days without enemy contact, my men would talk about how they missed the rush.
I was lucky enough to bring all of my men home from Afghanistan. Even now, two years later, we still joke about missing the firefights. Though I left the Marine Corps last month after nearly 10 years of service, I will still share with my men the memories of being pinned down in alleyways, the sound of bullets whizzing past our heads and the stench of death.