Beyond the Breaking Point
Caught between military occupation and separatist terrorism, a society that doesn't talk about mental health is desperate for psychiatrists, faith healers, medication — anything that could help heal "one of the most traumatized places on earth." A multimedia exclusive.

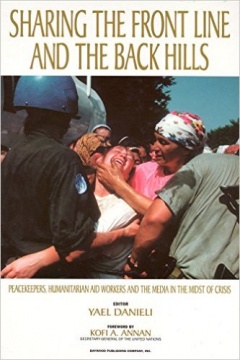
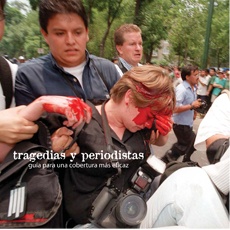
Kashmiri men seeking mental health support crowd the entrance of psychiatrist Arshad Hussain's clinic.
This project was partly funded by the South Asian Journalists Association.
In the space of 20 minutes, psychiatrist Arshad Hussain has taken a call on his cell phone from a suicidal patient and handed a box of pills to a woman who thinks her murdered brother follows her around. A former detainee, too scared to stay home alone, wants to consult with him, as does a widow who faints at the memory of her husband’s shooting. Meanwhile, several men desperate to refill their tranquilizer prescriptions are trying to barge into the office. Dr. Hussain, gesturing to a guard to bolt the door, apologizes to a visitor for not serving traditional Kashmiri tea. “It’s a bit busy today,” he says dryly.
In fact, it’s just a typical day. Last year, Dr. Hussain and his small staff received 100,000 visitors, most of whom exhibited classic symptoms of post-traumatic stress disorder: panic attacks, flashbacks and nightmares. Stories of American soldiers returning from Iraq with what used to be quaintly called shell shock are now growing familiar. Mercifully, those cases make up a small minority of the American population. Dr. Hussain is dealing with a problem on an entirely different scale. What happens when an entire society is suffering from PTSD?
That society is Indian-ruled Kashmir, thought by mental health experts to be one of the most traumatized places on earth. Nearly 20 years of separatist uprising and its brutal suppression has inflicted deep psychic wounds that continue to fester even though the worst of the violence has passed. At least 40,000 Kashmiri men of fighting age have died, and thousands of others have disappeared in the Indian crackdown on Islamic militants. Countless more youths have been picked up in random shakedowns. Bombs go off in public places. Ordinary civilians are caught between the two sides, fearing that their neighbors might betray them to either camp. The signs of the conflict are everywhere — coils of barbed wire on town bunkers, army convoys that populate major roads, soldiers standing guard in empty fields.
Practically everything that can cause PTSD has coalesced in Kashmir — loss, fear, distrust, random violence, a sense of powerlessness. The unrelenting Indian occupation fuels despair. Stress affects nearly everyone: the men routinely frisked on the street, the women forced to beg when their husbands vanish and the children given up to orphanages. Kashmir illustrates what researchers have long suspected: that prolonged exposure to direct confrontation results in still greater anguish. People don’t get used to violence; they grow more vulnerable. Under that pressure, the social networks that glue communities together crumble.
Kashmir’s extreme case raises troubling questions for conflict areas elsewhere. What happens to a generation born of collective trauma? Does PTSD beget more violence? Are “talk therapies,” recognized as effective in the West, the cure in a culture where people believe in ghosts?
Most importantly: how can an entire society be healed?
Not easily, says Kaz de Jong, a mental health advisor with MSF-Amsterdam, which operates a mobile clinic in an attempt to reach more remote areas. He estimates the prevalence of psychological distress in Kashmir at 33 percent, one of the highest rates in the world. (By comparison, the United States registers at 6 to 8 percent.) “The accumulation of events results in higher levels of distress,” de Jong explains. “What you see in chronic conflict is that self-support mechanisms and resilience go down.” Instead of getting stronger, the afflicted just get more desperate.
In the face of that desperation, patients endure hours in the hospital’s dirty halls for a five-minute audience in the presence of a dozen other patients and their accompanying relatives. This is not a population given to seeking treatment for psychiatric problems. In fact, mental illness carries a heavy stigma, which explains why most patients opt to see Dr. Hussain at the general hospital rather than the psychiatric ward. His resources are so stretched that some people get a single, cursory session, with little or no follow-up. The only thing in generous supply is medication, which the beleaguered staff hand out like Tootsie Rolls at Halloween.
Most of the people seeking help are women who were thrust into a breadwinning role when their men vanished. Doctors say the stress of trying to feed their kids often breaks them more than the initial loss of their mates.
Such is the case of Farida Sunderwani, 34, who suffers from headaches so bad that she rips out her hair. Grief after her husband died in crossfire turned to total collapse when her in-laws kicked her out of the house. Too weak to work, Sunderwani relies on handouts from neighbors. “I have no more dignity,” she states flatly.
The women in turn pass on their hopelessness to the next generation, and children are reporting to the psych clinic in greater numbers. So, too, are young men of fighting age, an unheard of development in a culture where males don’t normally admit to weakness. Even more surprising is the rise in suicides, especially among males.
“The Kashmiri language doesn’t have a word for suicide,” remarks Dr. Hussain. “That speaks volumes about the rarity of the phenomenon in this society. This is a Muslim society that used to have the lowest rate of suicide in India. But the past few years have seen a spurt of cut throats and burns.”
He fears that Abdur Rashid Kawdar could be next. Kawdar has wandered like a restless ghost ever since he found his brother’s body by the river. The throat was slit. Then soldiers killed a brother-in-law. Kawdar can’t hold down a job and visits the psychiatric clinic everyday, his eyes vacant without hope.
The antidote to this madness is elusive. Even if Dr. Hussain could offer all his clients proper counseling, Western psychotherapy’s focus on the individual often doesn’t work in traditional cultures such as Kashmir’s. What does work, says Jack Saul, a clinical psychologist who directs the International Trauma Studies Program in New York City, is engaging spiritual leaders and extended families to keep people from being cast out. Religion in particular can bind a person to a peaceful past and strengthen a sense of identity.
Dr. Hussain agrees. He prefers to see patients at their homes so he can reach them in the greater context of their communities. For instance, the primary concern of many women is taking care of their children, so he tries to connect mothers with charities that can help. Most importantly, he encourages traumatized Kashmiris to seek solace with faith healers and shrines.
“Spirituality acts as a buffer for trauma here,” he says. “We find fast track relief that way. Whatever was culturally appropriate before continues to be in the healing.”
At the shrine up the hill, a group of his patients take handfuls of blessed rock sugar and make wishes that their missing relatives will return. Then they wail out their pain in the comfort of company and slowly return home — with tranquilizers safely tucked in their pockets, just in case.